As a medical professional, you will likely come into contact with ECGs on a daily, if not hourly, basis. While ECGs are used to diagnose a wide range of medical issues, there are a few critical ECG patterns that you should be able to identify and interpret without any hesitation.
In this post, we’ll look at some common ECG patterns, what they mean for your patient’s health, and the typical treatments for each issue. You can also click here if you just want to skip the article and download our PDF cheat sheet.
Typical ECG Patterns You Should Be Familiar With
A medical provider’s ability to correctly interpret and react to an ECG could mean the difference between life and death for a patient. While not every condition that an ECG can alert you to will be a life-threatening one, there are a handful of ECG patterns that indicate a life-threatening event is either about to occur or is currently occurring.
Ventricular Fibrillation (VF)
Ventricular fibrillation is a condition where the heart’s lower chambers (the ventricles) beat in a very disorganized and erratic fashion. This condition is life-threatening, causing cardiac arrest if not treated immediately.
The ECG pattern for VF is characterized by a fast heart rate of more than 350 beats per minute, along with chaotic irregular deflections of varying amplitude, with no identifiable P waves, QRS complexes, or T waves.
VF often arises from ventricular tachycardia and is the most common cause of sudden cardiac death. While its underlying mechanisms are still not fully understood, it is generally thought to be caused by a combination of electrical and mechanical factors.
The electrical factors are thought to include abnormal myocardial ion channel function, changes in the cell-to-cell coupling, and abnormalities in cardiac autonomic nervous system function. The mechanical factors are thought to include myocardial ischemia, infarction, scarring, and changes in myocardial shape and size.
Treatment of ventricular fibrillation requires immediate defibrillation, a procedure that uses electrical shocks to stop the chaotic electrical activity and reset the heart’s rhythm. Once VF is terminated, then drugs, including antiarrhythmic agents may be used to prevent VF from recurring.
Other drugs may be used to treat other conditions like ischemia and a weak heart. Most of these patients also receive an internal cardiac defibrillator (ICD). This computerized device is implanted under the skin beneath the collar bone and wires run through the veins to the heart.
ICDs monitor the heart 24/7/365 for VF and ventricular tachycardia and immediately shock the heart out of it if detected.
Start Your Membership Today
We make electrocardiogram interpretation simple and understandable. The videos are interactive, and have detailed, easy to follow illustrations.
Ventricular Tachycardia (VT)
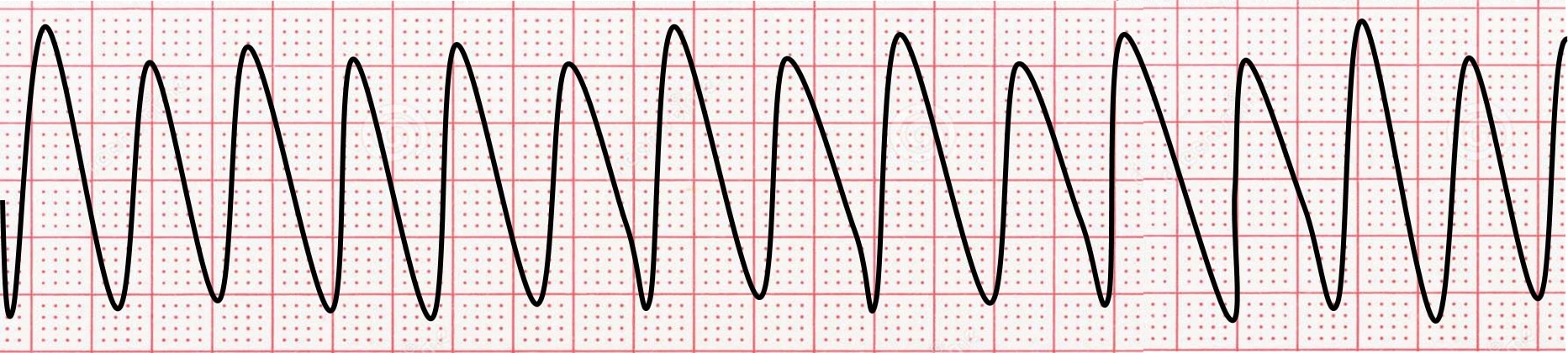
Ventricular tachycardia (Vtach) is when the heart’s lower chambers (the ventricles) beat too fast. This is a very serious condition that can lead to cardiac arrest.
The ECG pattern for VT is characterized by a fast heart rate typically between 100 and 250 beats per minute. Unlike ventricular fibrillation, the rhythm is more organized so distinct QRS complexes (beats) are seen on the ECG.
Heart rates over 150 beats per minute are often associated with symptoms, whereas Vtach slower than 150 bpm may be relatively asymptomatic. Vtach is a serious cardiac arrhythmia that occurs when the heart’s electrical impulses are not conducted properly. This can cause the heart to beat too fast, which can lead to a number of serious symptoms, including chest pain, shortness of breath, palpitations, dizziness, and passing out.
Vtach in itself is often life-threatening and needs urgent if not immediate treatment. Additionally, Vtach can degenerate to ventricular fibrillation and cardiac arrest, which is certainly lethal.
There are a number of treatment options available for Vtach. These include electrical cardioversion, which is a procedure that uses electric shocks to reset the heart’s rhythm, and defibrillation, which is a procedure that uses electric shocks to immediately stop the heart’s electrical activity and allow it to restart in a normal rhythm.
In some cases, medications may also be used to break Vtach, including antiarrhythmic medications that help regulate the heart’s rhythm and anti-ischemic agents that improve blood flow to the heart. Ultimately long-term medications are used.
Patients with ventricular tachycardia, like ventricular fibrillation, often receive an internal cardiac defibrillator to monitor their heart rhythms and shock the heart if Vtach is detected. With early diagnosis and treatment, the prognosis for Vtach is generally good.
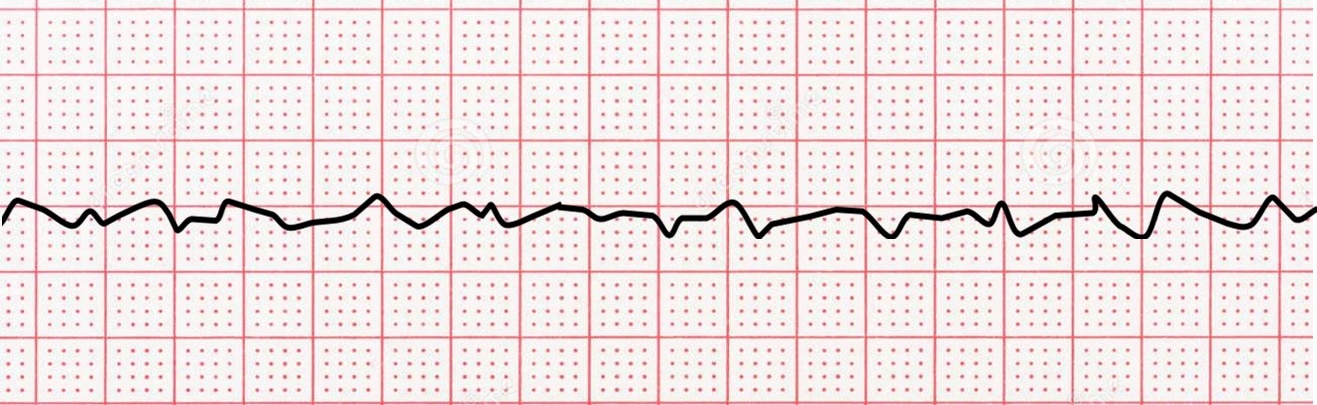
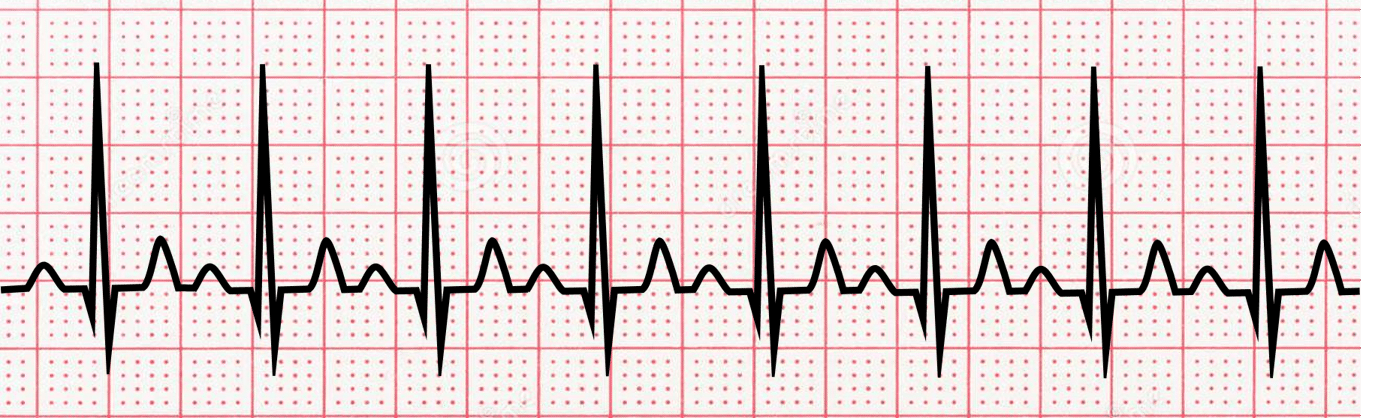
Atrial Fibrillation (AFib)
Atrial fibrillation is a condition where the heart’s upper chambers (the atria) beat in an irregular and disorganized fashion. This can lead to a number of symptoms, including chest pain, shortness of breath, palpitations, and dizziness.
The ECG pattern for AFib is characterized by an irregular heart rhythm and the presence of atrial fibrillatory waves. For simplicity, the ECG looks like a fine, squiggly, horizontal line, with irregular vertical complexes. Atrial fibrillation (AFib) is one of the most common types of arrhythmia and affects millions of people worldwide. Although it is generally not a life-threatening condition, it can lead to a number of serious complications, including stroke and heart failure. AFib is also a risk factor for sudden cardiac death.
Various risk factors, including high blood pressure, coronary artery disease, and diabetes, make patients prone to AFib. The best way to treat AFib is to prevent it from happening in the first place.
This can be done by avoiding triggers, such as alcohol, caffeine, and tobacco, as well as making sure that your risk factors are controlled. If AFib does occur, there are a number of treatment options available. One option is electrical cardioversion, which is a procedure that uses electric shocks to reset the heart’s rhythm
Medications are also used to treat AFib. These include agents that regulate the heart rate, or antiarrhythmic drugs that regulate the heart’s rhythm. Since patients with atrial fibrillation are at such a high risk of having a stroke, almost all receive blood thinners. With proper treatment, the prognosis for AFib is generally good.
Start Your Membership Today
We make electrocardiogram interpretation simple and understandable. The videos are interactive, and have detailed, easy to follow illustrations.
Supraventricular Tachycardia (SVT)

Supraventricular tachycardia (SVT) is a condition where the heart’s electrical impulses are conducted abnormally, causing the heart to beat too fast. Unlike ventricular tachycardia discussed above, the fast heart rhythm of SVT originates from the upper chambers of the heart and is typically not life-threatening.
The most common symptom is palpitations, but some patients may experience chest pain, shortness of breath, and lightheadedness. The ECG pattern for SVT is characterized by a rapid heart rate of more than 100 beats per minute. P-waves may be absent or may follow closely behind the QRS complexes.
If patients are markedly symptomatic or the patient’s blood pressures are too low, then immediate electrical cardioversion is done. This procedure shocks the heart allowing the electrical mechanism to reset to normal. Providers often recommend vagal maneuvers to terminate SVT.
These may include gentle pressure on the carotid arteries in the neck, asking the patient to bear down like having a bowel movement or even splashing cold water on the patient’s face. Certain medications will halt SVT, including beta-blockers, calcium channel blockers, digitalis, and adenosine.
Long-term solutions include medications and radiofrequency ablation of the SVT source. With proper treatment, the prognosis for SVT is generally good.
Sinus Tachycardia
Sinus tachycardia is a condition where the heart beats faster than normal. This can be caused by a number of things, including exercise, stress, anxiety, and certain medications.
The ECG pattern for sinus tachycardia is characterized by a regular heart rhythm and a heart rate of more than 100 beats per minute. There are normal P-waves and QRS complexes, but they occur faster than normal. Sinus tachycardia is seldom serious and always caused by some extenuating stimulus.
The key treatment for sinus tachycardia is finding the stimulus and treating it. For example, providers will treat the thyroid gland if it is overactive and stimulating the heart. Cardiac medications are rarely needed. In general, patients with sinus tachycardia have a good prognosis.
Start Your Membership Today
We make electrocardiogram interpretation simple and understandable. The videos are interactive, and have detailed, easy to follow illustrations.
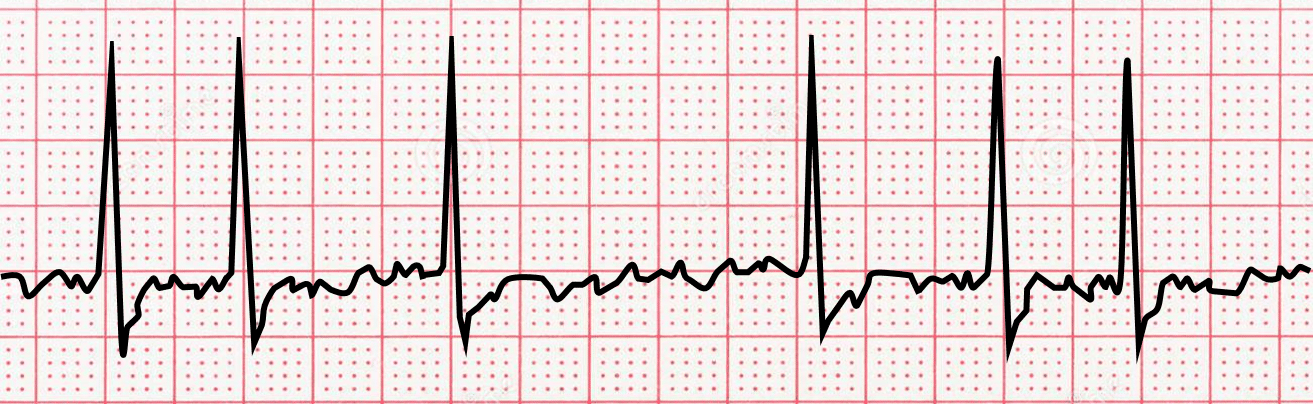
Sinus Bradycardia
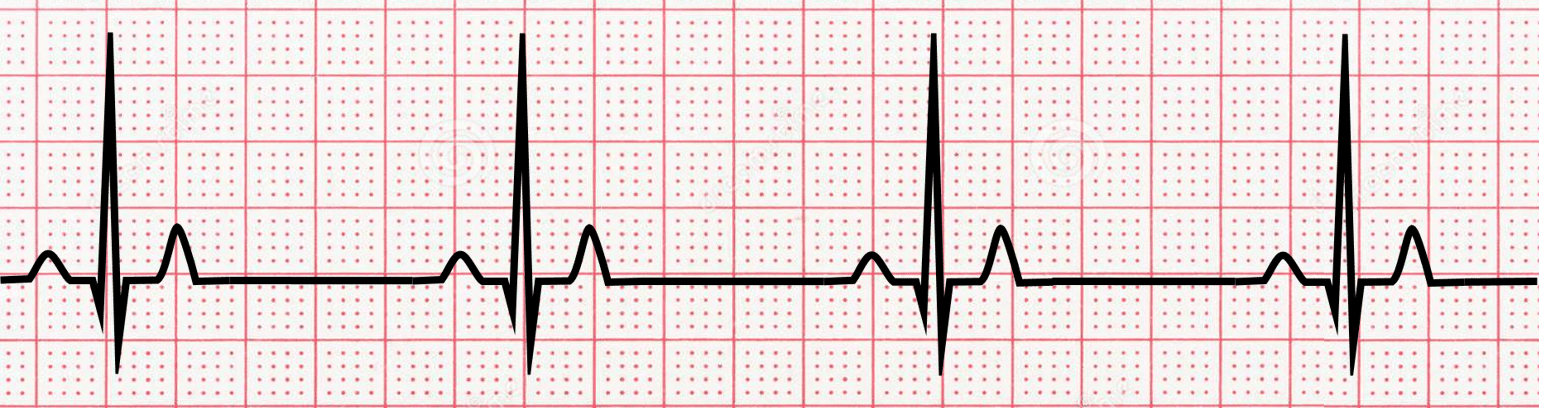
Sinus bradycardia is a condition where the heart beats slower than normal. This can be normal as in well-seasoned athletes, but can also be a sign of abnormal cardiac electrical activity. Additionally, several medications are notorious for causing bradycardia.
The ECG pattern for sinus bradycardia is characterized by a regular heart rhythm and a heart rate of fewer than 60 beats per minute. There are normal P-waves and QRS complexes, but they occur slower than normal. Mild sinus bradycardia is usually asymptomatic and benign.
Severe sinus bradycardia with heart rates below 50 beats per minute may be associated with shortness of breath, lightheadedness, or fainting. If sinus bradycardia is asymptomatic and the patient can perform a normal activity, then no treatment is needed. If the sinus bradycardia is caused by a medication then the medication should be adjusted or stopped.
Some patients with sinus bradycardia require a pacemaker to prevent the heart from going too slow. A pacemaker is a computerized device implanted under the skin, beneath the collar bone with wires that go to the heart through the veins.
How Can You Improve Your ECG Interpretation Skills?
To help with your identification of these common ECG patterns, click here to download our ECG pattern cheat sheet.
If you’re a medical professional or medical student that wants to improve your ECG interpretation skills, you should explore the Executive Electrocardiogram Education course catalog for the right ECG interpretation course for you.
We offer ECG interpretation courses for nurses, nurse practitioners, doctors, and just about every other medical professional that may need to read an ECG.
If you’re looking for the best possible deal, our ECG Premium Course includes access to all of our paid courses as well as practice ECGs. You can also sign up for our free ACLS rhythms course to get a feel for how our platform works.



