Our ECG interpretation course covers fundamentals and advanced topics in ECG interpretation and cardiac management.
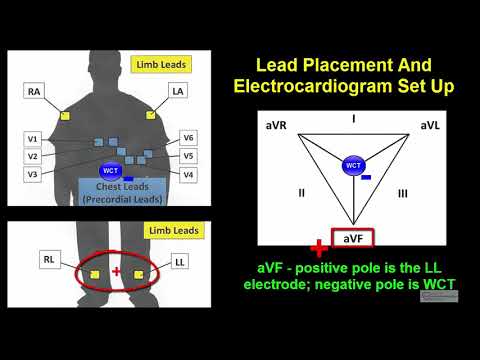
Electrocardiogram Fundamentals
Fundamentals of electrocardiogram interpretation include basic ECG waveforms, lead placement, and ECG axis determination. After this section, students will be able to set up and take basic ECG readings while identifying constituent components of the ECG waveforms.
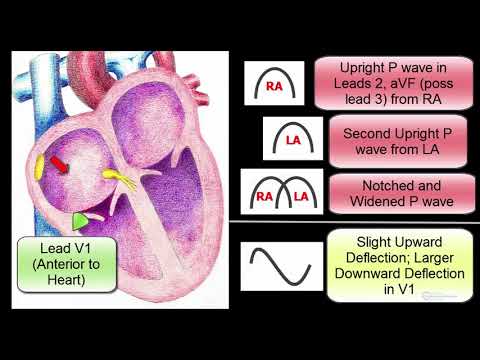
Atrial Abnormalities And Ventricular Hypertrophy
This section covers the ECG criteria for atria abnormalities and enlargement as well as the major ECG findings associated with left- and right ventricular hypertrophy. Students will learn about these conditions and how to recognize them easily on an ECG.
Bundle Branch Blocks and Fascicular Blocks
The section on bundle blocks and fascicular blocks concerns different types of impediments to electrical signaling in heart tissue. Students will cover left bundle branch blocks, right bundle branch blocks, incomplete bundle branch blocks, non-specific intraventricular conduction delays, as well as left anterior and left posterior fascicular blocks. By looking at the width of the QRS complexes and the QRS axis, you will easily identify these abnormalities.
Atrioventricular Blocks And Dissociation
Atrioventricular blocks come in three primary kinds:
- First-Degree
- Second-Degree (Mobitz Type I & II)
- Third-Degree or Complete Heart Block (CHB)
These blocks occur due to interruptions in electrical activity between the atria and ventricles. This section will also cover atrioventricular dissociation—ECG patterns in which atrial and ventricular activity do not correlate.
Ischemia, Injury, Infarction, and ST & T Wave Changes
Ischemia (loss of blood flow), physical injury, and infarction (heart muscle death) can all affect ECG tracings. This section covers the general pathophysiology of these conditions and how they affect the electrical signals in the heart. Specifically, students will learn how these conditions cause Q waves and changes in ST & T segments of the waveform.
Normal and Abnormal Rhythms
Normal and abnormal cardiac rhythms are detected on electrocardiograms. Rhythms are named by the area in the heart from which they originated and a description of the heart rate. Students will learn about:
- Sinus Rhythms: Rhythms originating from the sinoatrial (SA) node and typically consisting of P waves, QRS complexes, and T waves in succession.
- Atrial Rhythms: Rhythms that originate from one or more ectopic sites within the atria. Here the P waves look unusual, but the QRS complexes and T waves look normal. Sometimes these rhythms appear to have an irregular pattern.
- Junctional Rhythms: Rhythms that originate from the atrioventricular (AV) node. These rhythms typically lack P waves but have normal QRS complexes and T waves.
- Supraventricular Tachycardia (SVT): SVT typically refers to fast rhythms that originate from the atrioventricular (AV) node. The QRS complexes and T waves are usually normal. The P waves may be absent or may be inverted and seen just after the QRS complexes.
- Ventricular Arrhythmias: Rhythms that originate from ventricular tissue. Here, the QRS complexes are typically wide and bizarre-looking.
Additionally, students learn terms which include:
- Bradycardia: Heart rates slower than the intrinsic rate of depolarization of a particular cardiac tissue (e.g., Junctional bradycardia)
- Normal: Heart rates going at the intrinsic rate of depolarization of a particular cardiac tissue (e.g., Normal sinus rhythm)
- Accelerated: Heart rhythms traveling faster than the intrinsic rate of depolarization of a particular cardiac tissue but slower than 100 beats per minute (e.g., Accelerated idioventricular rhythm)
- Tachycardia: Heart rhythms between 100 and 250 beats per minute (e.g., Ventricular tachycardia)
- Flutter: Heart rhythms between 250 and 350 beats per minute (e.g., Atrial flutter)
- Fibrillation: Heart rhythms faster than 350 beats per minute (e.g., Ventricular fibrillation)
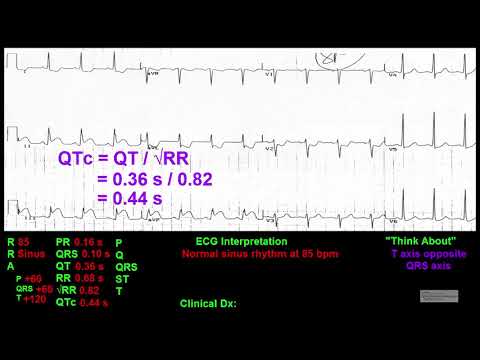
The QT Interval, Systemic Abnormalities, Electrolyte and Drug Effects, WPW, Lead Reversal, and Pacemakers
This section covers various abnormalities and systemic conditions that can affect an ECG reading. Things such as pacemakers, prescription drugs, and congenital abnormalities can all affect the cardiac conduction system and cause changes in an ECG. This chapter focuses on learning how one can identify these abnormalities via ECG readings.
Guidelines to ECG Interpretation and Practice ECGs
The last section contains a slew of practice ECG interpretation modules and guidelines on ECG interpretation. Learning the criteria is one thing, but this set of chapters explains the step-by-step approach that cardiologists use to read the ECG. All ECGs are interpreted from start to finish, and you will learn to read like this. Learning this systematic approach increases your ECG reading accuracy and provides the best patient care ever. Students will be able to take the skills in lectures and apply them to practical situations.