Ventricular tachycardia and ventricular fibrillation are two serious cardiac arrhythmias that can often lead to death. Because of the critical nature of these abnormal heart rhythms, it is essential to be able to identify each on an ECG or rhythm strip.
In this article, we’ll cover the differences between Vtach and Vfib, as well as the causes, risk factors, treatments, and what each looks like on an ECG.
What Is Ventricular Tachycardia?
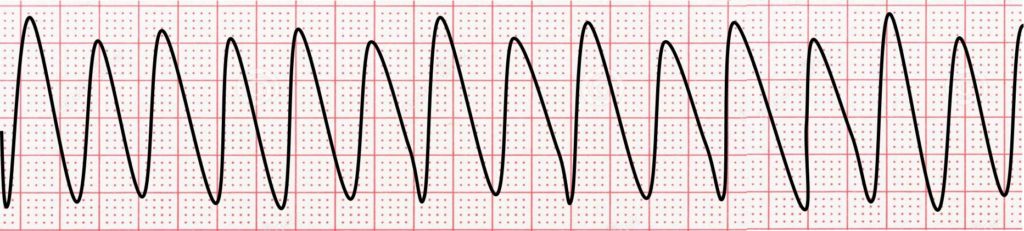
Ventricular tachycardia (V-tach or VT) is an abnormal heart rhythm that originates from a single ectopic site within the ventricle (lower chamber of the heart). The heart rate is typically between 100 and 250 beats per minute, and V-tach replaces the normal heart rhythm that begins in the SA node. Because the impulses start in the ventricles and do not follow the normal electrical “highway” within the heart, the QRS complexes are wide and bizarre-looking rather than narrow and normal.
Vtach can result in unstable blood flow, causing low blood pressure. In some cases, VT can degenerate into ventricular fibrillation and cardiac arrest. Ventricular fibrillation is discussed in more detail below. In general, diagnosing V-tach on an ECG is easy. It should be considered in any patient with a history of heart disease presenting with a wide-complex tachycardia on their ECG.
VT has several classifications. One is based on the duration, and one is based on the morphology or form of the QRS complexes. Sustained V-tach lasts longer than 30 seconds, while nonsustained V-tach lasts shorter than 30 seconds. With monomorphic V-tach, all wide, bizarre QRS complexes look the same. With polymorphic V-tach, the wide, bizarre QRS complexes look different. Regardless of these classifications, all may be symptomatic.
Ventricular Tachycardia Risk Factors
Ventricular tachycardia has a few risk factors. Patients may be at a higher risk for Vtach if they have existing heart issues, take certain medications (especially those that prolong the QT interval), and more. The following factors will increase their chance:
- Damage to the heart from a heart attack
- Myocarditis or inflammation of the heart muscle
- Cardiomyopathies causing a weak heart or thick heart muscle
- Congestive heart failure
- Valvular heart disease
- Certain medications (e.g., digoxin and many more) or street drugs
- Congenital heart disease leading to structural defects
- Congenital heart disease of the conduction system like prolonged QT syndrome or Brugada’s syndrome
- Electrolyte imbalances like severe lack of magnesium in the blood
- Hypertension
What Causes Vtach?
While ventricular tachycardia’s causes are often unknown, several factors can contribute to the development of Vtach, and understanding these causes is essential for proper diagnosis and treatment. One of the primary causes of Vtach is underlying heart conditions, such as coronary artery disease, cardiomyopathy, or a previous heart attack that has left scar tissue in the ventricles. These conditions can disrupt normal electrical conduction within the heart and create an environment that is more susceptible to abnormal heartbeats.
Typically, other pre-existing heart conditions will cause Vtach such as:
- Congestive heart failure resulting in an inability to pump blood properly
- Cardiomyopathy, a condition resulting in heart muscle issues
- Arrhythmogenic right ventricular dysplasia, a hereditary heart disorder
- Structural heart disorder (congenital or acquired)
- Drug toxicity from specific medications or street drugs
- Electrolyte imbalances, like hyperkalemia, hypokalemia, and hypomagnesemia
- Myocarditis, an inflammation of the heart muscle
Proper identification and management of these potential triggers is crucial for reducing the risk of Vtach and maintaining overall cardiac health.
How Ventricular Tachycardia Is Treated
Treatment for ventricular tachycardia varies widely depending on the severity and whether it is symptomatic. The primary goal of treatment is to restore a normal heart rhythm, prevent future episodes, and address any underlying conditions that may be contributing to Vtach. Standard treatments include:
- Vagal maneuvers: Coughing, tensing the body, and activating the gag reflex are commonly recommended vagal maneuvers.
- Anti-arrhythmic medications: Medications to stabilize the patient’s heart rhythm can be very effective.
- Blood pressure medication: These do not directly treat the VT but reduce this risk factor’s effect.
- Cardioversion: Applying a controlled shock to the heart to reset it to a normal heart rhythm.
- Defibrillation: Applying an emergent shock to the heart to reset it to a normal heart rhythm.
- Internal Cardiac Defibrillator (ICD): A device implanted under the collarbone with wires that go into the heart to allow for constant cardiac monitoring and shock therapy if needed.
What Is Ventricular Fibrillation?
Ventricular fibrillation (Vfib) is also an abnormal heart rhythm originating from the ventricles. Instead of coming from one oversensitive focus, it originates from many hypersensitive ventricular sites. As such, the electricity in the ventricles goes mad, and 350-600 small jolts are given off each minute.
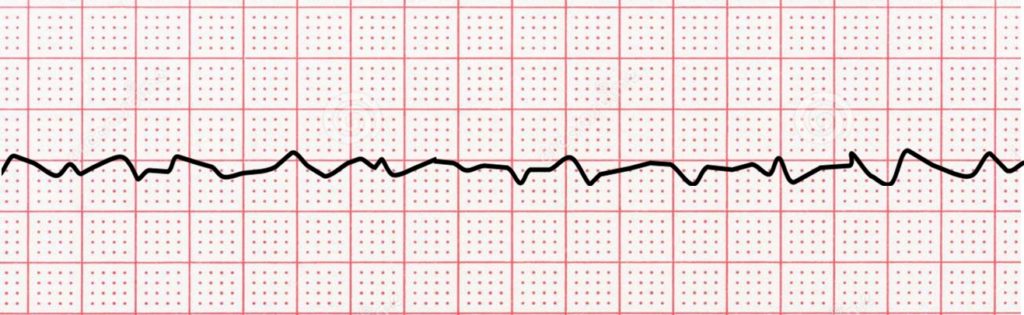
As you might imagine, this dysfunctional electrical mechanism is so chaotic that the ventricles just quiver and do not beat effectively, resulting in no blood flow in the body. The ECG displays this chaotic electrical activity as a fine squiggly horizontal line.
Without immediate treatment, ventricular fibrillation usually results in cardiac arrest. Most cases of Vfib result from a heart attack, and in some cases, ventricular tachycardia may precede it.
What Are the Risk Factors for Ventricular Fibrillation?
Again, the risk factors for ventricular fibrillation are the same as those for ventricular tachycardia. Risk factors that are more common are those that cause damage or weakening of the heart muscle. These conditions also make patients vulnerable to congestive heart failure. Foreign substances such as stimulants and illegal drugs like cocaine make people susceptible. Finally, people who have had V-tach or Vfib in the past are more likely to have them again.
What Causes Vfib?
The causes of ventricular fibrillation are the same as ventricular tachycardia (see list above). It occurs due to underlying structural cardiac insults, electrical cardiac issues, or systemic abnormalities. As noted above, Vfib is most associated with acute myocardial infarctions (heart attack), but many other conditions can cause it.
How Vfib Is Treated
Emergent cardiac defibrillation is the treatment for ventricular fibrillation. Defibrillation involves shocking the heart as quickly as possible to try to restore a normal rhythm. While waiting for a defibrillator, cardiopulmonary resuscitation (CPR) is done to try to maintain the circulation of blood in the body.
In an outpatient setting, find an automatic external defibrillator (AED), place it on the unconscious person’s chest suspected of having Vfib, and follow the instructions. The machine will let you know if a shock is indicated.
Treating the underlying conditions that caused the Vfib is also necessary. If the patient suffers a heart attack, then consider medicines and stenting. If the patient is septic, then treat the infection. If the magnesium level is low, then supplement. Certain medications, including antiarrhythmic agents, may be used. Eventually, patients who develop ventricular fibrillation need an internal cardiac defibrillator implanted.
What Does Ventricular Fibrillation Look Like on an ECG?
Ventricular fibrillation shows no clear P waves, T waves, or QRS complexes on an ECG, and the rate may be up to 600 beats per minute. Because the heartbeat is erratic from struggling to pump blood, deflections will vary in amplitude and usually decrease as time goes on. Vfib looks like a thin squiggly line without organized complexes. It can be course, as in the rhythm strip below, or be fine, appearing almost straight.
The Clinical Significance of Vfib
Ventricular arrhythmias are more likely to interrupt the pumping of blood or undermine the heart’s ability to supply the body with oxygen-rich blood. This makes ventricular fibrillation a clinically significant event, frequently resulting in loss of consciousness or even death.
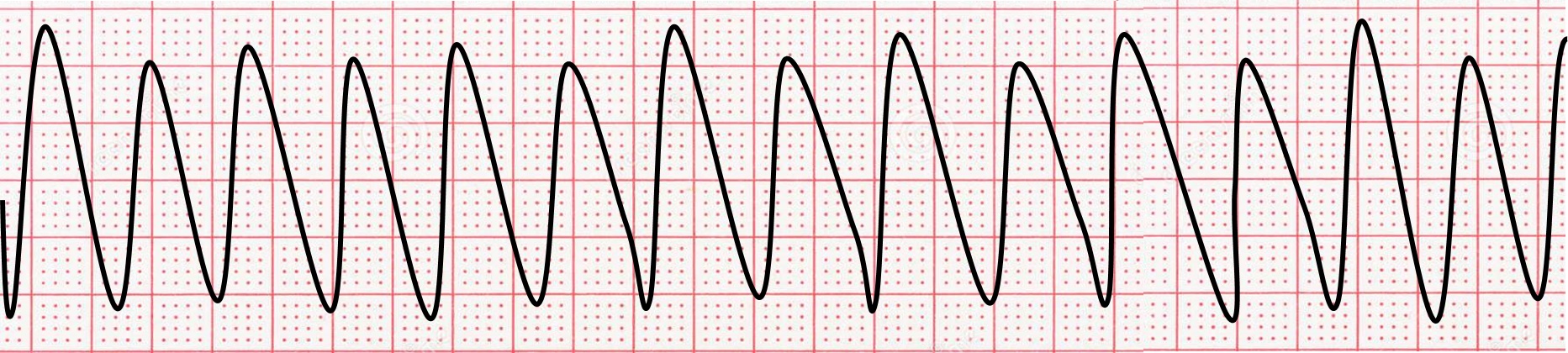
What Does Ventricular Tachycardia Look Like on an ECG?
Since ventricular tachycardia is a rhythm that originates from an abnormal single focus in the ventricles, it does not follow the normal conduction pathways. As such, instead of the QRS complexes looking thin and normal, they are wide and bizarre-looking, just like premature ventricular complexes. The QRS complexes are usually greater than 120 ms (3 small boxes in duration). Tachycardia refers to heart rates over 100 beats per minute (100-250 bpm). Subsequently, V-tach looks like lots of wide complex beats, one-after-another at a rate between 100 and 250 beats per minute.
With monomorphic VT, all of the QRS complexes look alike. With polymorphic VT, the QRS complexes look different. Sometimes an independent rhythm from the atria is seen marching through the QRS complexes.
ECG Characteristic of Ventricular Tachycardia on an ECG
Certain characteristics of the QRS complexes give clues that the beats come from the ventricle instead of the normal conduction pathway. They include:
- Concordance of the QRS complexes in the chest leads (all of the complexes are upright or all of the complexes are downward)
- QRS complexes are > 0.14 seconds wide
- AV dissociation
- Fusion and capture beats
- A superior QRS axis
- Monophasic R wave in V1
- Specific QRS complex morphologies in lead V1
- If the QRS complexes are upright in V1:
- Monophasic R wave, qR pattern, rS pattern, Rr’ pattern.
- If the QRS complexes are downward in V1:
- Notched S wave, R wave > 30 ms wide, late nadir > 60 ms.
- If the QRS complexes are upright in V1:
The Clinical Significance Of Vtach
The significance of V-tach often depends on the heart rate. If the V-tach is less than 150 beats per minute, circulation in the body may be maintained, and oxygen-rich blood may flow normally. These patients may be asymptomatic. Due to the fast heart rate, though, some patients feel palpitations. Effective circulation is often lost if the V-tach goes at rates greater than 150 beats per minute. Patients may feel palpitations and may feel faint. They can pass out or die, regardless of the symptoms. V-tach needs to be treated urgently. Remember that V-tach can degenerate into Vfib.
Learn More About ECG Interpretation On ECGEDU.com
Executive Electrocardiogram Education offers a variety of course offerings that will help you learn to interpret ECGs like a veteran, including being able to identify the differences between ventricular tachycardia and ventricular fibrillation.
Our online ECG courses are designed for just about any medical professional, including doctors, med students, nurse practitioners, nurses, EMTs, and more. You can learn more about each of our courses on our course pricing page or contact us today if you have questions about which of our ECG interpretation courses might be best for you.