My patient complained of palpitations. I ordered a 24-hour Holter monitor. Nothing is more frustrating than receiving a report stating “arrhythmias seen, no diary submitted,” and then finding out from the patient that they were never asked to even keep a diary during monitoring. From my perspective, the patient’s time and money, as well as my time, have been wasted. What should a provider expect from a Holter reading? This article outlines proper setup, patient instructions, and reading guidelines for Holter monitoring.
What Are Holter Monitors and Why Order Them?
Holter monitors are portable electrocardiographic (ECG) devices used to record heart rhythms. A typical Holter monitors heart rhythms for 24-48 hours. During this time it records every beat. Patients keep a diary to allow correlation of symptoms to the heart rhythm. One may order a Holter monitor to look for arrhythmias as a cause of palpitations, passing out (syncope), or lightheadedness (near syncope), shortness of breath (dyspnea), or fatigue. In addition, a Holter may help discover the cause of chest pain, the risk of cardiac events related to congenital heart diseases, or lastly, to assess the efficacy of cardiac treatment.
What Are Palpitations?
Before further discussing Holter monitors, let us first talk briefly about palpitations. Palpitations are the feeling that the heart is beating out of sync. Patients may describe racing, fluttering, skipped beats, a flip-flop sensation, the heart-stopping, and many other feelings. The symptom may be in the chest, back, abdomen, throat, or neck. They may be brief or prolonged, sudden or insidious. Regardless, patients feel them. Cardiac rhythm monitors help to decide if the palpitations arise from an arrhythmia or non-cardiac etiology.
Try Our ACLS Rhythm Course For Free!
This course goes through all of the ACLS rhythms. You will be quizzed on each rhythm and then watch the detailed description which points out the salient features.
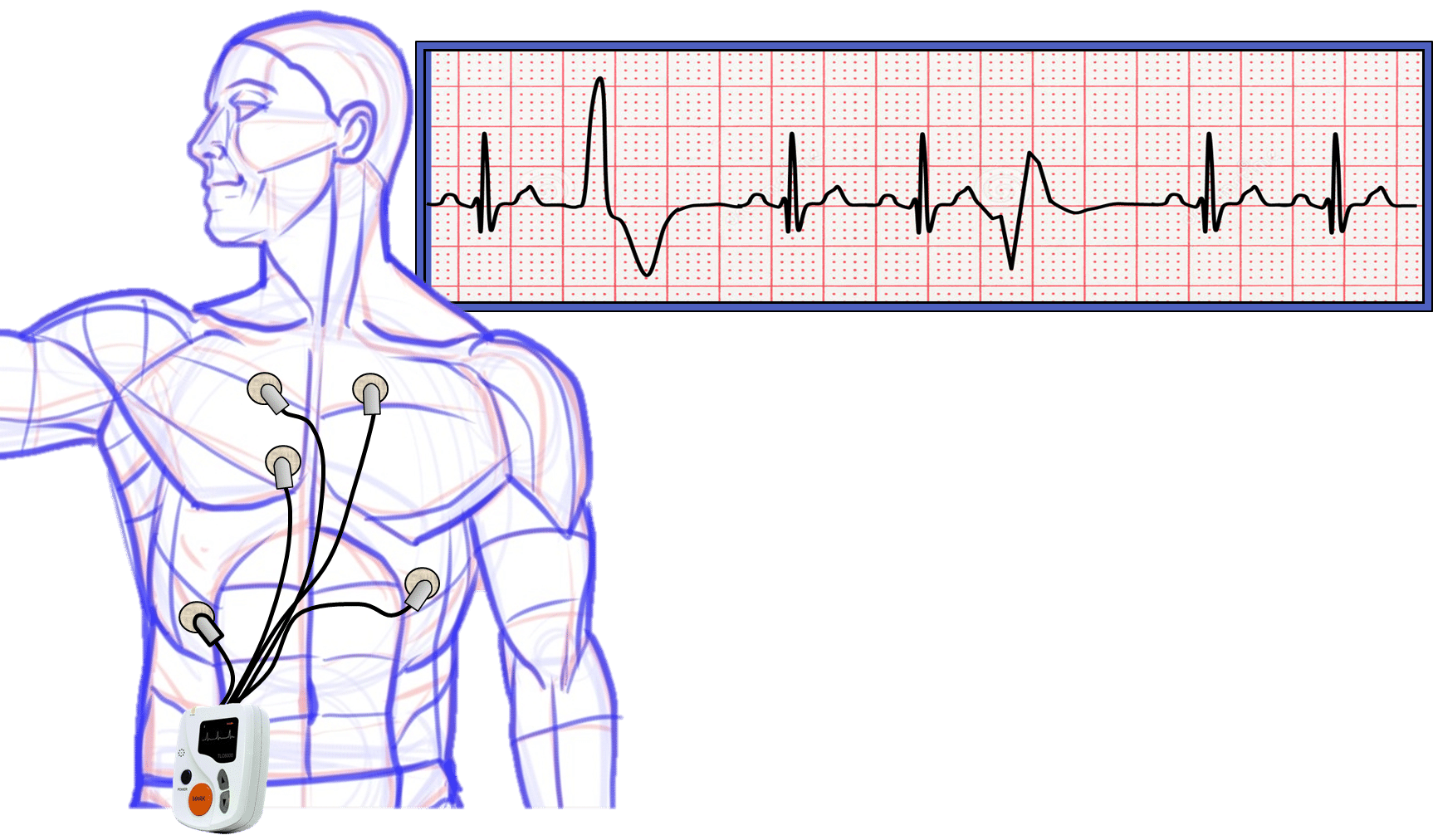
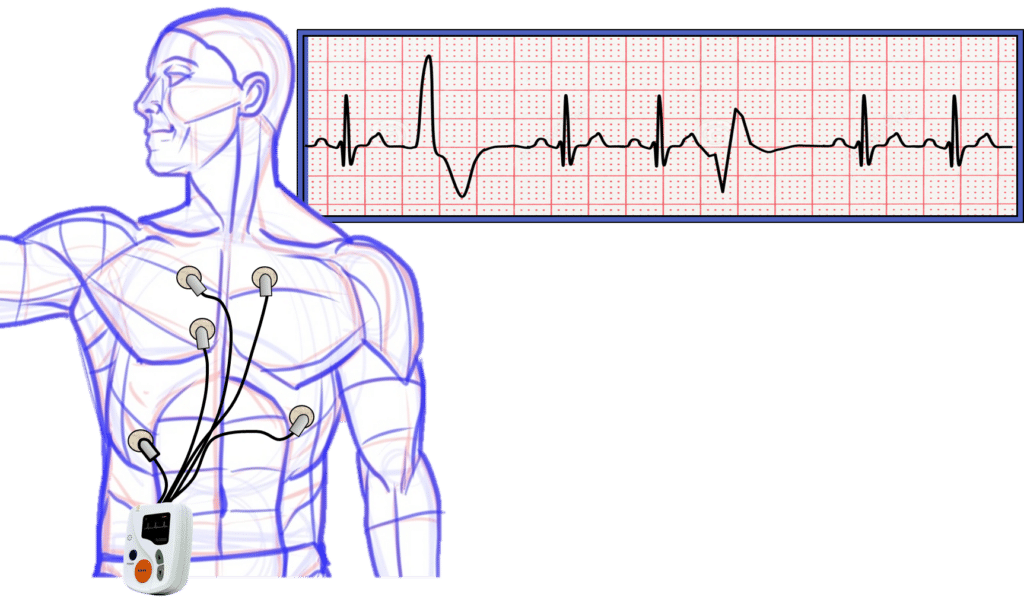
Holter Set-Up
Setting up the Holter monitor is simple. The technician, or patient, stick electrodes to the chest, attach one end of wires to the electrodes and attach the other end of the wires to the monitoring unit. The patients then receive instructions to keep a diary. For simplicity, the diary has three columns. The time of day goes in the first column, the patient’s activities go in the second column, and the patient’s symptoms go in the third column. Clinical information is paramount to an accurate Holter reading.
Holter Processing
Once the monitoring company/office receives the unit back, they process the information. A technician, with the help of a computer, analyzes each beat and series of beats. Additionally, the technician enters times, activities, and symptoms from the patient diary. This allows the proper correlation of symptoms to arrhythmias or other abnormalities.
Holter Reading
Five basic components go into a good Holter reading. They include the underlying rhythm, ectopy, or abnormalities, from the ventricles, ectopy from the atria, ST and T wave changes, and finally patient symptoms with a correlation to Holter findings. Additionally, I state how long monitoring occurred and the start date of the Holter.
Underlying Rhythm
The underlying rhythm is important. Is it sinus or atrial fibrillation or even a pacemaker rhythm? Regardless, it lets the ordering provider know the patient’s baseline. The Holter reader should also state the average, minimum and maximum heart rates.
Ventricular Ectopy
Is there ventricular ectopy? Ventricular ectopy is described as single beats (premature ventricular complexes), double beats (ventricular couplets), triple beats (ventricular triplets), and ventricular runs. In general, rare arrhythmias occur <1% of the time. Occasional arrhythmias occur 1-5% of the time and frequent arrhythmias occur >5% of the time. The reader also records runs of ventricular ectopy such as non-sustained ventricular tachycardia. The reader should also comment on the maximum length and maximum rate of the runs.
Try Our ACLS Rhythm Course For Free!
This course goes through all of the ACLS rhythms. You will be quizzed on each rhythm and then watch the detailed description which points out the salient features.
Atrial Ectopy
Similar to ventricular ectopy, atrial ectopic beats and rhythms are reported. Atrial ectopy is also described as single beats (premature atrial complexes), double beats (atrial couplets), triple beats (atrial triplets), and atrial runs. Again, rare arrhythmias occur <1% of the time. Occasional arrhythmias occur 1-5% of the time and frequent arrhythmias occur >5% of the time. Here again, the reader records runs of atrial ectopy. Runs may include paroxysmal atrial tachycardia, atrial flutter, atrial fibrillation, multifocal atrial tachycardia, and other forms of supraventricular tachycardia. Significant episodes of bradycardia are also recorded. The reader should also comment on the maximum length and maximum rate of the runs.
ST and T wave changes
Some Holter monitors have the ability to analyze ST and T wave changes. This is important when assessing a patient for signs and symptoms of coronary artery disease. For example, is there ST-segment elevation correlating to times that the patient complains of chest pain? Is there new T wave inversion at the same time as inappropriate bradycardia? Is there ST-segment depression associated with sinus tachycardia during exercise? All three of these examples may indicate cardiac ischemia prompting further evaluation of the patient’s coronary arteries.
Symptoms and Correlations
Correlation of Arrhythmias to the Time of the Day
Knowing the patient’s activities during the day help correlate appropriate and inappropriate heart rhythms. For example, a heart rate of 38 beats per minute is abnormal at 3:00 p.m. unless the reader knew that the patient naps at this time. Similarly, a sinus tachycardia of 150 beats per minute is abnormal at 2:00 a.m. unless the reader knew this patient exercises at this time and is not sleeping.
Correlation of Arrhythmias to Symptoms
Symptoms need to be correlated to arrhythmias. Additionally, the reader should mention when symptoms do not correlate with any abnormalities. For example, are the palpitations concurrent with premature ventricular complexes, or is the patient’s rhythm normal?
Start Your Membership Today
We make electrocardiogram interpretation simple and understandable. The videos are interactive, and have detailed, easy to follow illustrations.
Example of an Appropriate Holter Reading
- 24-hour Holter performed beginning 1/1/2021.
- Underlying sinus rhythm with average heart rate 75 beats per minute (range 43 – 162 beats per minute).
- Frequent (8%) premature ventricular complexes; Rare (<1%) ventricular couplets and triplets; Four short runs of non-sustained ventricular tachycardia (maximum run 7 beats at 150 beats per minute); One, 10-minute episode of accelerated idioventricular rhythm at 78 beats per minute; No long ventricular runs.
- Occasional (2%) premature atrial complexes; Rare (<1%) atrial couplets; Twenty-three short runs of paroxysmal atrial tachycardia (maximum run 14 beats; maximum rate 150 beats per minute). No episodes of atrial fibrillation.
- One (1) millimeter ST-segment elevation occurring during sinus tachycardia at 3:00 p.m. Heart rate was 152 beats per minute. ST-segment elevation lasted until the sinus tachycardia resolved at 3:05 p.m. No other significant ST or T wave changes noted.
- The heart rate response was appropriate to the time of day and activities noted in the diary. Palpitations overall correlated to premature ventricular complexes. No symptoms reported at times of non-sustained ventricular or atrial tachycardia. Symptoms of “flutters” were associated with sinus rhythm. Complaint of “chest pressure” correlated with sinus tachycardia and ST-segment elevation.
Conclusion
Holter monitors, or any tests for that matter, are tools to help confirm or exclude a suspected diagnosis. As most Holter monitors are obtained due to symptoms like palpitations, it is incumbent upon the staff, monitoring company, and Holter reader to follow all of the necessary steps. The monitor must be placed correctly. The patient must keep a diary. The company/office must analyze and record the symptoms. And finally, the interpreter must list all of the normal and abnormal findings and correlate symptoms.