In the fast-paced world of modern medicine, accurate and timely diagnosis is vital for effective patient care. ECG pattern recognition and differential diagnosis are important tools that allow healthcare professionals to identify potentially life-threatening conditions such as arrhythmias, ischemic heart disease, or electrolyte imbalances before they develop into critical situations.
From understanding basic ECG patterns to unraveling the various arrhythmias, coronary heart disease, and heart attacks, this comprehensive guide will enlighten you on the importance of ECG pattern recognition and differential diagnosis in modern medicine.
Understanding Differential Diagnosis And ECG Pattern Recognition
ECG pattern recognition helps diagnose and monitor various heart conditions. By analyzing the heart’s electrical activity through the P, QRS, and T waves, physicians can detect abnormalities and determine the extent of damage to the heart muscle. This information is important for making informed decisions about treatment plans and effectively managing patients’ symptoms, which is where differential diagnosis comes in.
Differential diagnosis is a medical diagnostic procedure in which doctors list possible conditions that could be causing a patient’s symptoms. This list isn’t the final diagnosis but is a starting point for further investigation and testing.
If a patient shows symptoms that match more than one condition, a differential diagnosis helps narrow down the possible causes by ruling out certain conditions through additional testing. The doctor then uses this information to create a list of possible disorders that have similar symptoms.
Additional tests, such as laboratory tests or imaging studies, may be ordered to narrow the list further and ultimately make the most accurate diagnosis.
The Importance Of ECG Pattern Recognition In Diagnosing
As a non-invasive diagnostic tool, an ECG records the heart’s electrical activity, providing valuable information about heart rate, heart rhythm, and the timing of electrical impulses as they travel through the heart’s various chambers. Pattern recognition can help physicians detect and diagnose cardiac arrhythmias, ischemic heart disease, electrolyte imbalances, and structural heart disease.
Identification Of Cardiac Arrhythmias And Abnormalities
Cardiac arrhythmias are irregular heart rhythms that can manifest as a heartbeat that’s too slow, fast, or irregular. ECG pattern recognition helps diagnose these abnormalities by allowing doctors to measure the timing and duration of each electrical phase of the heartbeat. This information helps them determine the nature of the arrhythmia and develop an appropriate treatment plan.
Training in advanced ECG interpretation techniques allows healthcare professionals to accurately identify these complex patterns associated with certain conditions while reducing the number of false positives or negatives.
Diagnosis Of Ischemic Heart Disease
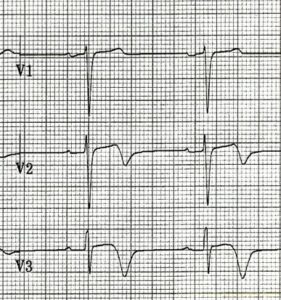
Ischemic heart disease occurs when the heart’s blood supply is blocked or interrupted by an accumulation of fatty substances and cholesterol plaques. A 12-lead ECG is a commonly used diagnostic method for patients with suspected ischemic heart disease.
By examining the ECG patterns, physicians can detect signs of myocardial ischemia, injury, or infarction. This information is important for confirming or ruling out unstable ischemic heart disease and persistent myocardial ischemia.
The classic pattern for ischemia on the ECG is isolated symmetrical T wave inversion in 2 or more contiguous leads. Contiguous means that the leads are anatomically near each other. Other signs of myocardial ischemia or injury may be T-wave flattening or ST-segment depression. Acute myocardial infarctions are recognized by ST-segment elevation, particularly in a patient presenting with classic cardiac chest pain. If the myocardial infarction affects the full thickness of the heart muscle then Q waves develop.
Detection Of Electrolyte Imbalances
Electrolyte imbalances can also affect the heart and lead to abnormal ECG patterns.
High potassium causes classic peaked T-waves, whereas low potassium flattens and widens the T-waves. Elevated serum calcium shortens the QT interval by shortening the ST segment. With hypocalcemia, the QT interval lengthens because of lengthening of the ST segment. Hyperkalemia, hypokalemia, and hypomagnesemia can cause dangerous arrhythmias.
Recognizing these patterns allows healthcare professionals to diagnose and treat the underlying electrolyte imbalance to prevent further complications.
Diagnosing Structural Heart Disease
Structural heart disease, such as ventricular hypertrophy, atrial septal defects (a hole between the upper chambers of the heart), arrhythmogenic right ventricular cardiomyopathy, and others refers to physical abnormalities in the heart structure. Certain ECG patterns can explain structural abnormalities and should be recognized.
An ECG may show left or right ventricular hypertrophy, indicating a thickened ventricle due to increased pressure overload.
Healthcare professionals must therefore have specialized training to accurately recognize these diagnostic patterns and distinguish them from other cardiac conditions.
Commonly Seen ECG Patterns
As a healthcare professional, it’s important to take the time to become familiar with common ECG patterns and their impact on patient health. Recognizing specific ECG patterns helps medical professionals distinguish between different heart conditions and accurately diagnose the issue.
Normal Sinus Rhythm
A normal sinus rhythm is a regular heartbeat that occurs at a reasonable rate. When interpreting ECGs, it’s important to recognize this type of heart rhythm as it can help distinguish between normal and abnormal rhythms.
When examining a patient’s electrocardiogram, healthcare professionals should look for P-waves preceding a QRS complex and observe a consistent PR interval within 120-200 milliseconds.
Sinus Bradycardia
Sinus bradycardia is a common ECG pattern with a heart rate of less than 60 beats per minute. This condition occurs when electrical signals generated by the sinoatrial (SA) node, the heart’s natural pacemaker, are transmitted at a slower pace than usual.
Electrical signals generated by the SA node travel through the heart’s conduction system, causing the atria and ventricles to contract in a coordinated manner. This process ensures efficient blood circulation throughout the body, but when the electrical signals are transmitted more slowly, the heart rate decreases, leading to sinus bradycardia.
It’s important to note that sinus bradycardia may be a normal physiological response in certain individuals, such as athletes or the elderly, during sleep. In these cases, the slow heart rate doesn’t indicate an underlying heart problem and isn’t considered a cause for concern.
Sinus Tachycardia
Sinus tachycardia is a heart rhythm that beats faster than normal, usually at more than 100 bpm, and shows normal P-waves, followed by normal, narrow QRS complexes. Various factors, including stress, anxiety, fever, dehydration, or physical exertion, can trigger this accelerated heartbeat.
In most cases, sinus tachycardia isn’t dangerous and often resolves on its own without needing a doctor to intervene. Sinus tachycardia is always caused by the body responding to outside factors. The outside factors may be benign, like exercising, but may be a clue to more serious problems like sepsis (a severe infection) or an overactive thyroid gland.
There are several other possible conditions characterized by a fast heart rate with a narrow QRS complex on an ECG. These include supraventricular tachycardia, atrial fibrillation, and atrial flutter, among others. With these conditions, the rhythm does not originate from the sinus node so the P-waves will look abnormal or be absent.
An assessment algorithm is performed to help determine the cause of the increased heart rate to aid in the sinus tachycardia diagnosis. This algorithm takes into account several factors, including the patient’s medical history, symptoms, and the results of diagnostic tests such as ECG, blood tests, and imaging studies.
Atrial Fibrillation
Atrial fibrillation (AFib) is a common cardiac arrhythmia with an irregular and rapid heart rhythm. It occurs when the electrical signals in the heart’s atria become chaotic, resulting in irregular and uncoordinated contraction of the atrial muscles. This condition can cause blood to pool in the atria (upper chambers of the heart), increasing the risk of blood clots, and strokes.
The ECG pattern of atrial fibrillation is clear, making it typically easy to diagnose. There are no visible P waves representing depolarization of the atrium; instead, the ECG may show coarse fibrillatory waves or no atrial activity at all. The QRS complexes that represent ventricular depolarization appear irregularly irregular with varying R-R intervals.
These irregular QRS complexes, and hence irregular pulse and rhythm, are due to the intermittent conduction of atrial action potentials through the AV node to the ventricles. The ventricular rate in atrial fibrillation is typically between 80 and 180 beats per minute but may be slower if the patient is taking medications to block the nodus AV, such as beta-blockers or non-dihydropyridine calcium channel blockers.
The main symptom of atrial fibrillation is palpitations, however, some patients display shortness of breath, decreased exercise capacity, fatigue, fainting, or feeling faint.
The differential diagnosis of atrial fibrillation involves distinguishing it from other abnormal heart rhythms such as atrial flutter, multifocal atrial tachycardia, sinus tachycardia with frequent ectopy.
Ventricular Tachycardia
Ventricular tachycardia (VT) is a potentially life-threatening condition characterized by a rapid, regular heartbeat originating in the heart’s ventricles. It can be caused by various factors, including structural or functional abnormalities of the heart, myocarditis, electrolyte imbalances, heart attacks, a weak heart, and drug-induced QT prolongation.
On the ECG, ventricular tachycardia appears as a series of wide, bizarre-looking QRS complexes at a rate greater than 100 beats per minute.
The differential diagnosis of ventricular tachycardia includes supraventricular tachyarrhythmias with aberrancy, fast pacemaker rhythms, inappropriate pacemaker rhythms, Wolff Parkinson White syndrome, and possibly coarse ventricular fibrillation. Ventricular tachycardia is serious and often life-threatening. It is a leading cause of sudden cardiac death. VT can accompany acute heart attacks and other cardiac conditions, therefore a careful history and physical exam of the patient is essential.
Bundle Branch Blocks
Bundle branch blocks (BBBs) are a common ECG finding. It’s an abnormality that results in widened QRS complexes. There are two main types of BBB: the right bundle branch block (RBBB) and the left bundle branch block (LBBB).
The medical significance of BBB varies from person to person and ranges from benign to potentially life-threatening cardiac conditions.
The differential diagnosis of BBB includes any condition that can widen the QRS complexes. These may include ventricular rhythms, some electrolyte abnormalities, and certain aberrant rhythms.
Killer ECG Patterns And Differential Diagnosis
Some ECG patterns, called “killer” patterns, indicate severe cardiac disease that requires immediate attention and intervention. Recognizing killer ECG patterns and performing a thorough history and physical examination, checking other tests if necessary, and then forming a comprehensive differential diagnosis is important to identify life-threatening heart disease and initiate appropriate treatment.
ST-Segment Elevation of an Acute Myocardial Infarction
In a patient presenting with acute substernal chest pain, you should get an immediate ECG to look for changes of an acute ST-segment elevation myocardial infarction (STEMI). The major clue is ST-segment elevation in 2 or more contiguous leads. This indicates a blockage in one of the blood vessels that supply the heart with oxygen and nutrients.
ST-segment elevation in leads V1 through V4 may indicate occlusion of the left anterior descending artery (LAD). This vessel typically supplies blood to 60% of the heart, and a blockage here can be devastating. ST-segment elevation in leads V5, V6, 1, and aVL may indicate a blockage in the circumflex artery, which supplies the left lateral portion of the heart. Finally, ST-segment elevation in leads 2, 3, and aVF, may indicate blockage in the right coronary artery (RCA), which supplies the inferior wall and posterior wall of the left ventricle as well as the right ventricle.
ST Segment Depression of Myocardial Injury or Ischemia
ST-segment depression in a patient presenting with chest pain may also be a sign of a heart attack, or unstable angina. If damage to the heart muscle occurs this is referred to as a non-ST-segment myocardial infarction (NSTEMI). These ECG changes also indicate blockages in the arteries that supply the heart with blood.
Although ST-segment depression is not specific to certain areas of the heart, your differential diagnosis should include stenosis or occlusion to any major or minor cardiac artery.
Wellins Syndrome Pattern
One critical ECG pattern that should not be missed by any practitioner is the Wellens Syndrome pattern. This pattern, typically seen in leads V2 and V3, has slight ST-segment elevation, followed by a deep inverted T-wave.
The main differential diagnosis is severe stenosis (narrowing) of the proximal left anterior descending artery. Remember as noted above, the LAD supplies 60% of the heart’s blood supply. Occlusion of this artery usually results in death and a blockage here is often referred to as the “widow-maker” lesion.
The Pattern Of ST-Segment Elevation In Acute Pericarditis
ST-segment elevation may also indicate various conditions, including acute pericarditis. Patients with acute pericarditis typically present with sharp chest pain and diffuse ST-segment elevation across multiple leads on the ECG.
The extent of ST-elevation is generally moderate, ranging from 0.5 to 1 mm. It’s important to note that ECG patterns may vary depending on the stage and cause of a patient’s pericarditis. For example, individuals with chronic constrictive pericarditis may have ‘domed’ T-waves instead of elevations due to prolonged inflammation and fibrosis in the pericardium.
In addition to pericarditis, other conditions associated with ST-segment elevation include:
- Myocarditis
- Stress cardiomyopathy (Takotsubo)
- Benign early repolarization
- Acute vasospasm
- Spontaneous coronary artery dissection
- Left bundle branch block
- Various channelopathies
- Electrolyte abnormalities
Accurate interpretation of these ECG patterns is necessary for proper diagnosis and treatment.
ECG Pattern Recognition Techniques
Electrocardiography has significantly advanced in recent years, particularly in recognizing ECG patterns. These methods have been developed to improve the accuracy and efficiency of ECG interpretation so medical professionals can better diagnose and treat various cardiac conditions.
The Steps Involved In ECG Interpretation
ECG interpretation involves analyzing the heart’s different waves, segments, and intervals in an electrocardiogram. The main steps of ECG interpretation are:
- Proper Electrode Placement: Place the ECG electrodes at specific locations on the patient’s chest, arms, and legs to ensure accurate data collection.
- Identify Heart Rates: Count the number of beats across the ECG and then multiply by 6. This works since most standard ECGs record the heart rhythm for 10 seconds.
- Assess the Rhythm: Analyze the ECG rhythm to determine if it’s regular or irregular and identify any abnormalities, such as premature beats or pauses.
- Evaluate P-Wave Morphology: Examine the shape and duration of the P-wave to determine if it’s normal or abnormal.
- Measure PR Interval: Measure the distance between the onset of the P-wave and the onset of the QRS complex to assess atrioventricular conduction delay.
- Analyze the QRS Complexes: Examine the duration, width, and amplitude of QRS complexes to detect ventricular depolarization abnormalities.
- Examine ST-Segment Elevation/Depression: Analyze ST-segment deviation from baseline to diagnose myocardial ischemia or injury.
- Evaluate T-Wave Morphology: Look at the T-waves’ morphology (shape) to detect repolarization abnormalities in conditions such as myocardial ischemia or hypokalemia.
- Determine Axis Deviation: Calculate axis deviation by evaluating leads I and AVF in a standard six-limb lead system used in electrocardiography analysis.
A more comprehensive system includes:
- Analyze the rate, rhythm, and axes.
- Analyze the intervals (PR, QRS, and QT).
- Analyze the ECG waves in order and in detail.
- P-waves, Q-waves, QRS complexes, ST-segments, and T-waves.
- List the ECG diagnoses.
- Make clinical diagnoses.
Understanding The Underlying Electrophysiological Disturbances
To truly understand ECG pattern recognition and differential diagnosis, it’s important to know the underlying electrophysiologic abnormalities that can cause abnormalities in an electrocardiogram.
For example, if a portion of the heart muscle isn’t receiving adequate oxygen due to blocked or narrowed coronary arteries, which can occur in conditions such as angina or acute myocardial infarction, there will be an imbalance between oxygen supply and demand. This can result in changes in the ST segment.
Similarly, certain cardiac arrhythmias, such as ventricular tachycardia, can disrupt normal electrical conduction in the heart and cause abnormal QRS complexes on ECG recordings.
Enroll In An ECG Interpretation Course Today
Whether you’re a nurse, doctor, or other healthcare professional, mastery of ECG pattern recognition and differential diagnosis is necessary to recognize and treat cardiac emergencies quickly and accurately. ECGEDU’s courses cover electrocardiogram basics, abnormal ECG patterns, and arrhythmia recognition. With interactive videos, easy-to-follow illustrations, and hands-on practice tests, you’ll become an ECG expert at your own pace.
Sign up for our ECG interpretation course today and unlock your full potential in electrocardiography.