Why Should You Be Able To Identify Common ECG Errors?
Even though computerized electrocardiogram (ECG) interpretations are fairly reliable, they still do not obviate the need for human confirmation.1 In the setting of technical or set up errors, the computer should never be expected to come up with the correct diagnosis. Every person who interprets electrocardiograms should know and identify the most common electrocardiogram errors and artifacts. This, in turn, will prevent patient misdiagnoses. This article goes through the most common ECG errors and artifacts, and details which electrocardiogram abnormalities should catch your attention.
Case Example
I recently saw a 40-year-old-man in cardiology consultation for a new anterior wall myocardial infarction on his electrocardiogram. The interpretation was made by the computerized ECG machine. The patient had no cardiac risk factors, was asymptomatic and exercised regularly. He was very confused by this ECG and did not know how he could of had a heart attack without even knowing it. When I looked at the electrocardiogram, leads V1 through V4 did not look right. I then realized that leads V1 and V3 were misplaced and simply switched in position. This gave the appearance of tall R wave in lead V1 and a Q wave in lead V3. The computer, not knowing any better, read out an anterior wall myocardial infarction.
Identifying Errors and Arm Lead Reversal
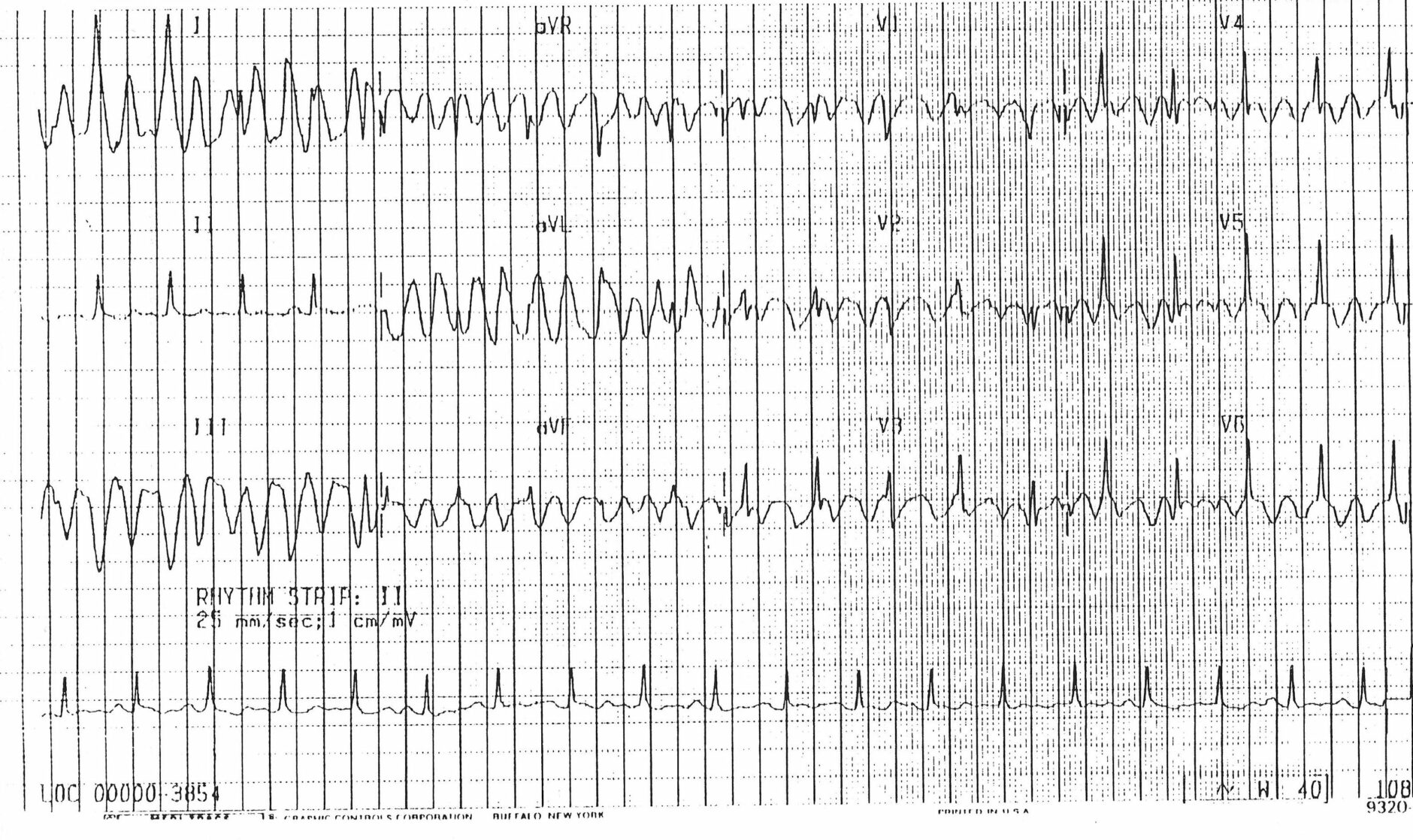
The most common technical problem is arm lead reversal.2 I am not sure why this happens, but even the most experienced electrocardiogram technicians make this mistake occasionally. The most obvious clue to the ECG reader is noticing right axis deviation of the QRS complex. Right axis deviation of the P waves and T waves is also present. Ultimately, if you compared an ECG with right-arm/left-arm lead reversal to a normal ECG then lead 1 will look upside down, leads 2 and 3 will look as if switched around, and leads aVL and aVR will look like they, too, switched places. aVF will appear the same on the new and old ECG.
Above: Abnormal ECG showing arm lead reversal
Identifying Errors and Arm/Leg Lead Reversal
Leg and arm lead reversal is far less common and is more difficult to recognize. Most of the time, the new and old electrocardiograms need to be compared to identify this setup error. So, if your new electrocardiogram looks very different from an old electrocardiogram and there is not a logical reason, consider arm/leg lead reversal and repeat your ECG.
Identifying Errors and Lead V2-V3 Reversal
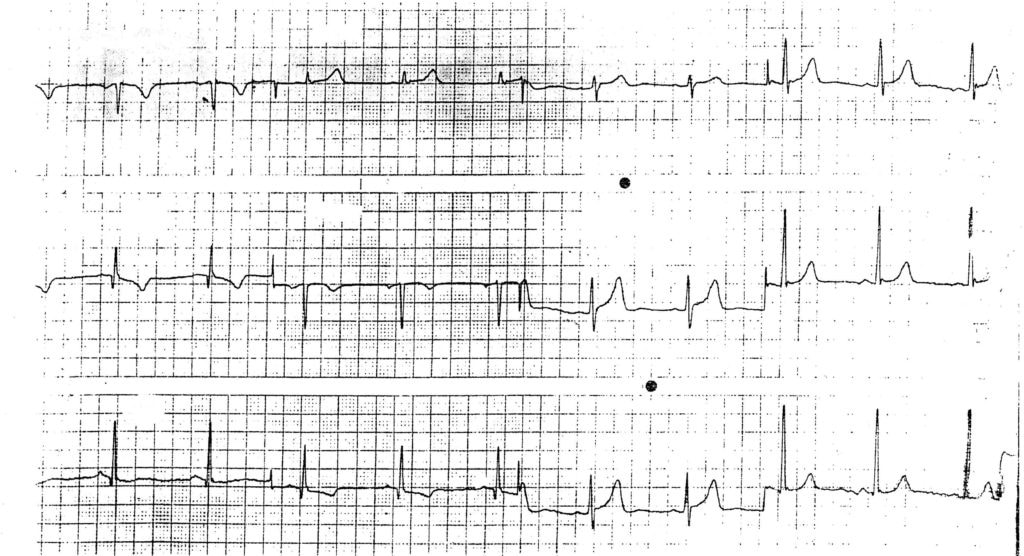
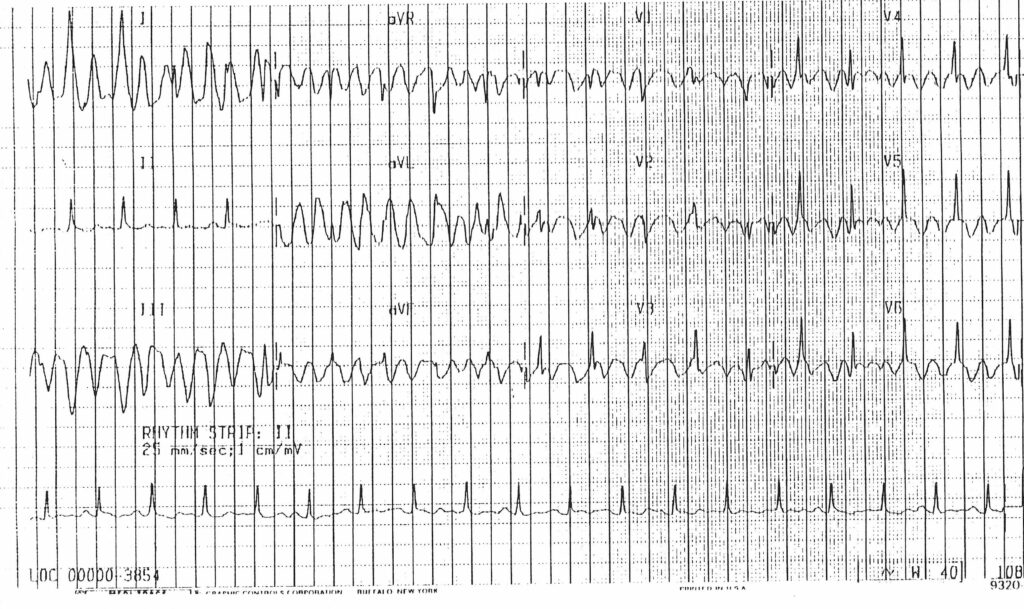
Another common lead reversal error is V2-V3 reversal.2 This will give similar results as with the patient I described above. Instead of the R wave starting small in V1 and getting bigger as you move toward V4, V5 and V6, the R wave is small, gets bigger and then smaller again. This is referred to as R wave reversal, which can suggest an anterior wall myocardial infarction. When you are looking at your ECG, make sure that the R waves get bigger going from lead V1 through V4, V5, and V6, and the S waves get smaller going from lead V1 through V6.
Above: Abnormal ECG showing reversal of leads V1 and V3
Identifying ECG Artifacts
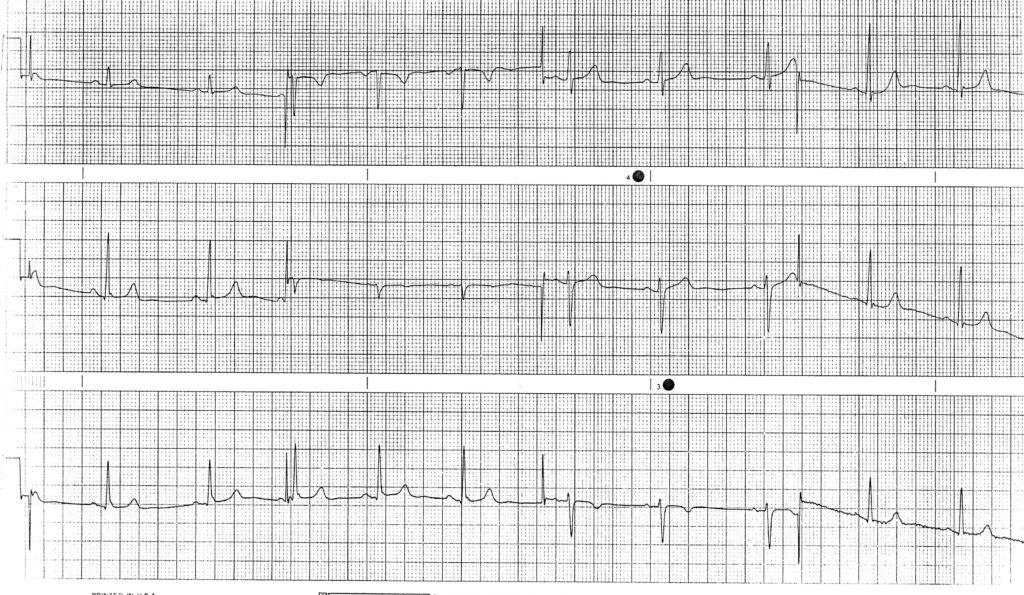
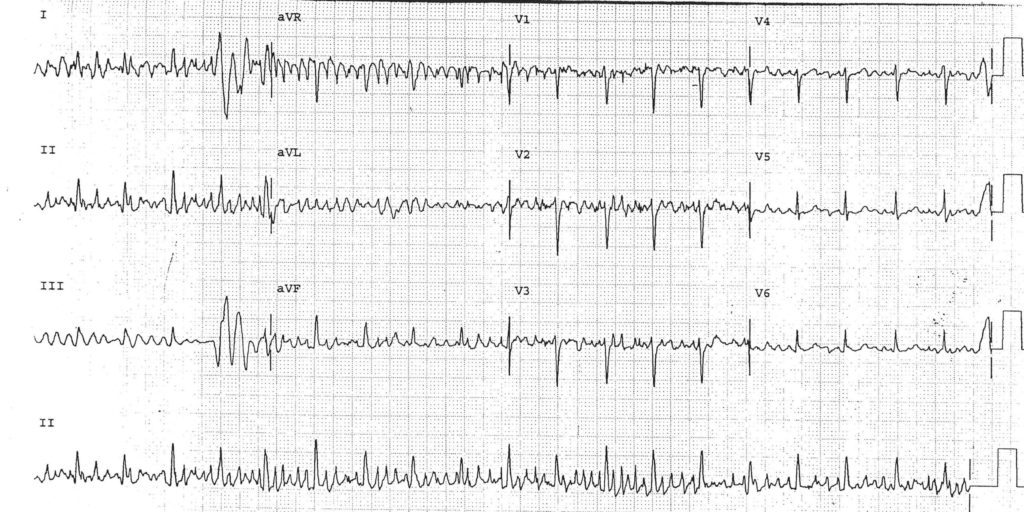
Electrocardiogram artifacts commonly lead to misdiagnosis. Artifacts can be caused by movement, electrical interference or altered filter settings.2 Artifacts from movement can make the baseline wander (fluctuate up and down), can give a small squiggly baseline that obscures true P waves and can give the impression of atrial flutter or fibrillatory waves. Sometimes the artifact can produce large regular waveforms that look like ventricular tachycardia. Excluding atrial fibrillation or flutter can sometimes be challenging, but if the QRS complexes are perfectly regular and you know the patient has a tremor such as from Parkinson’s Disease, then baseline artifact should be considered. If you see large waves that look like ventricular tachycardia, then you should try to find a regular rhythm that is going through these waves. Since a patient cannot have sinus rhythm and ventricular tachycardia at the same time, then the extra wave must be artifactual.
Above: Abnormal ECG showing baseline artifact in a patient with tremors from Parkinson’s Disease
Above: Artifact is seen throughout this ECG. In some leads, this artifact looks like ventricular tachycardia
Identifying Artifact by ECG Machine Filters
Electrocardiogram machines assign filtering to electrocardiograms depending on the specific circumstances. For simplicity, filters eliminate unwanted artifact and noise. The two main filters used are high-pass and low-pass filters. High-pass filters reduce low-frequency noise, such as motion artifact, respiration variation and baseline wander.2,3 Low-pass filters remove high-frequency noise, such as muscle artifact and external interference like electrical interference.2,3 Low-pass filtering has a noticeable affect on the QRS complex, epsilon, and J-waves, but does not alter repolarization signals.3 The filter settings are typically displayed at the bottom of the electrocardiograms and should be looked at every reading.
ECG Machine Filter Settings
High-pass filters can be set between 0.01-1.0 Hz. The higher the high-pass filter is set (e.g. 0.5 Hz), there are more chances of seeing changes or distortion of the ST segments.3 Low pass filters are set between 40-150 Hz. The lower the low-pass setting, the more muscle and electrical artifact is removed. Unless there is a lot of these artifacts, a higher low-pass setting (e.g. 150 Hz) can be used.3 An optimal settings on the average ECG is 0.05 – 150 Hz (high-pass 0.05 and low-pass 150) for full fidelity ST-segments and late potentials.3 Understanding filtering is far more complex than described here, but should at least be thought about when seeing significant changes on different ECGs of the same patient.
Computer Error vs. Human Error
Lastly, I review a study that looked at a comparison of the computerized electrocardiogram interpretation compared to that of cardiologists. It concluded that: “The most frequent errors in computer ECG interpretation [were] related to arrhythmias, conduction disorders, and electronic pacemakers. Computer ECG diagnosis of life threatening conditions (e.g. acute myocardial infarction or high degree AV blocks) [were] frequently not accurate (40.7% and 75.0% errors, respectively).”4 Based on this, computerized electrocardiogram interpretations need to scrutinized. When I teach electrocardiogram interpretation, I suggest that students read the electrocardiogram independently. Then look at the computerized interpretation and go through the diagnoses one-by-one and figure out why they agree with or refute these diagnoses. They should ask, “Why did the computer come up with each diagnosis? What criteria did the ECG machine use? If it is wrong, why and what criteria will I use?”
Conclusion
In conclusion, ECG readers need to be able to identify errors and artifacts. These can be due to mistakes with ECG setup, due to intrinsic electrocardiogram machine settings or outside interference. Misdiagnoses could lead to patient harm and can be avoided.
Scott L. Siegal, D.O., FACOI
Cardiologist
12/22/2018
References
1Electrocardiograms, Family Physician Interpretation (Position Paper), (2017 December BOD), Amer Academy of Fam Practioners (AAFP).
2García-Niebla J, Llontop-García P, Valle-Racero JI, Serra-Autonell G, Batchvarov VN, and de Luna AB. Technical mistakes during the acquisition of the electrocardiogram. Ann Noninvasive Electrocardiol. 2009 Oct;14(4):389-403. https://en.ecgpedia.org/wiki/Technical_Problems
3Whatford, C. Understanding ECG Riltering. (2014 March 10). EMS-Topics. www.ems12lead.com/2014/03/10/understanding-ecg-filtering/.
4Guglin ME, Thatai D. Common errors in computer electrocardiogram interpretation. Int J Cardiol. 2006 Jan 13;106(2):232-7. https://www.ncbi.nlm.nih.gov/pubmed/16321696