An ECG is one of the most efficient and most effective tests to evaluate the heart, making ECG interpretation a vital diagnostic skill in any medical setting. ECGs are used when diagnosing a wide range of heart issues, including myocardial infarction, ventricular fibrillation, or bundle branch blocks.
An ECG is comprised of 12 leads that are broken down into two sets – chest leads and limb leads. Each lead analyzes the same electrical events; they’re just capturing the data from different angles.
This article will cover some of the basics that you should know about 12-lead ECGs, what they measure, and what you’ll need to know before learning to interpret ECGs.
How the 12-Lead ECG Works
The 12-lead ECG works by recording the heart’s electrical activity through ten electrodes placed across the patient’s body. Each lead captures the activity and outputs it as a waveform on a screen or piece of paper.
ECG leads are either bipolar, composed of two electrodes of opposite polarity, or unipolar, a lead with a single positive electrode and a reference point. The standard 12-lead ECG consists of three bipolar limb leads, three unipolar limb leads, and six unipolar chest leads.
Electrodes
ECG electrodes are pads that attach to the skin, conduct electricity and connect to the ECG machine to generate the 12 leads that detail the patient’s heart activity. While there are 12 leads, there are only ten electrodes.
With a standard 12-lead ECG, six chest electrodes and four limb electrodes adhere to the skin. Each electrode must be placed properly because if not, you may capture incorrect data, which could result in a misdiagnosis. You can learn more about proper lead placement in this article.
Leads
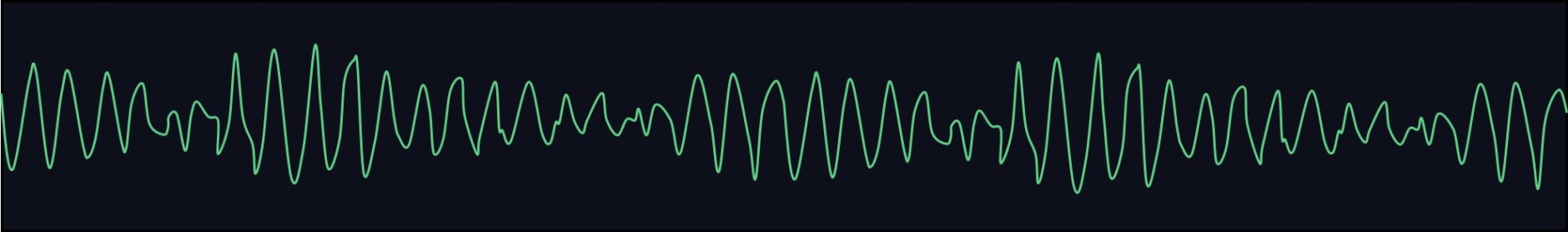
Leads are not the pads that attach to the patient’s body, but they are the 12 perspectives of information the ECG machine records. The ECG machine writes this information in constant waveforms that a healthcare provider can interpret. As the patient’s heart beats, the electrodes allow the electricity to flow to the machine.
What Are the 12 Monitored Leads?
As we’ve mentioned, an ECG is comprised of 12 leads from ten electrodes that attach to the patient’s limbs and chest to provide information from the heart. Limb electrodes attach anywhere on the patient’s left and right arms and legs, while the placement of the chest electrodes is more specific.
Limb Leads
Limb leads look at the heart’s electrical activity in a vertical direction. The limb leads specifically look at the coronal axis, the inferior myocardium, and the high lateral myocardium. Additionally, the heart rhythm can be easily identified from the limb leads. As noted above, Leads I, II, and III are bipolar leads and have a positive and a negative electrode. aVR (augmented vector right), aVL (augmented vector left), and aVF (augmented vector foot) are unipolar leads and use a common reference point called Wilson’s Central Terminal as the negative point.
Limb leads offer a vertical display of the heart and include:
- Lead I: This lead looks at the heart from the left side. The positive electrode is on the left arm, and the negative electrode is on the right arm.
- Lead II: This lead looks at the heart from the bottom left. The positive electrode is on the leg, and the negative electrode is on the right arm.
- Lead III: This lead looks at the heart from the bottom right. The positive electrode is on the leg, and the negative electrode is on the left arm.
- Lead aVR: This lead looks at the heart from the upper right. The positive electrode is on the right arm.
- Lead aVL: This lead looks at the heart from the upper left.
- Lead aVF: This lead looks at the heart from the bottom.
Chest Leads
Chest leads offer a horizontal perspective from which to look at the heart, and these leads provide lateral, anterior, septal, and posterior views. The six chest leads are relatively easy to remember as they have names from one to six.
Like the Augmented Vector Leads (aV_ leads), the chest leads use Wilson’s central terminal as a reference point. The chest leads begin on the right side of the sternum and wrap around the left side of the chest. Shaving any hair on the patient’s chest before placing electrodes can help you get a more accurate reading.
- V1: This lead is placed in the fourth intercostal space on the right side of the sternum.
- V2: This lead is placed in the fourth intercostal space on the left side of the sternum.
- V3: This lead is placed directly between V2 and V4.
- V4: This lead is placed in the fifth intercostal space in the midclavicular line.
- V5: This lead is placed in the fifth intercostal space in the anterior-axillary line.
- V6: ThThis lead is placed in the fifth intercostal space in the mid-axillary line.
Leads V1 and V2 look at the intraventricular septum and the posterior wall. Leads V3 and V4 visualize the anterior left ventricular wall. Leads V5 and V6 see the lateral left ventricular wall.
Each lead of an ECG is like looking at the heart from a different vantage point. Subsequently, each lead has a unique shape to its waves. The electrocardiogram machine assigns each lead to an assigned section of the ECG paper.
What Is the ECG Measuring?
The heart’s electrical activity originates from the sinoatrial (SA) node, which is the heart’s intrinsic pacemaker. The sinus node is located in the upper right of the heart. The ionic flow travels through the atria (upper chambers of the heart) into the atrioventricular (AV) node (area of the heart separating the electrical system between the atria and ventricles) and then into the ventricles (lower chambers of the heart). This electrical current travels to the lower left of the heart.
The ECG shows a flat, horizontal line when the cells are in steady state (e.g., no electrical activity). The ECG machine sees electrical changes as the ions move in and out of the cardiac cells. The first wave on the ECG is the P-wave. P waves look like little bumps. P-waves represent depolarization of the SA node, atria, and AV node.
A short flat line follows this as the electricity prepares to travel into the ventricles. Next, are larger deflections called QRS complexes. These waves represent depolarization of the ventricles. Another short, flat line occurs, followed by another wave, called a T-wave. T waves depict repolarization of the ventricles.
The ECG records the rates at which the electrical impulses travel through the heart. Specific intervals measured are the PR interval, the QRS interval, and the QT interval. The PR interval looks at the time from the onset of the impulse in the SA node through the AV node. The QRS interval measures the time of conduction from the AV node through the bundles, Purkinje fibers, and the rest of the ventricles.
Other alterations in the waveforms give other information about cardiac conditions. For example, tall QRS complexes may represent left or right ventricular hypertrophy (thickening of the heart muscle). Q waves suggest a heart attack, and ST-segment and T wave changes might reflect other injuries to the heart.
What Aspects of the ECG Are Interpreted
During an ECG interpretation, the electrical activity helps you interpret vital information about the patient’s heart activity. Depending on the shape of a waveform, you can determine the direction the current travels in and how much electricity flows in each direction. If the current isn’t flowing as it should, it may indicate health issues for the patient.
The ECG machines display impulses a certain way. Impulses traveling toward an electrode give a positive or upright deflection on the ECG graph. Impulses traveling away from an electrode show a negative or downward deflection. Impulses that go perpendicular to the electrode exhibit a flat line or an isoelectric waveform. Isoelectric waves have small upward and downward deflections. Since ECG waveforms display both direction and magnitude, they are vectors.
ECG Waves
ECG readers learn how to interpret the heart’s electrical activity. Positive and negative deflections represent the average direction of the electrical current’s travels. By comparing the normal wave activity of a healthy patient to the results of another patient, you can determine whether that patient needs further tests or treatment or if their current heart health is normal for their age.
Depending on the angles, directions, and magnitude of ionic flow toward and away from electrodes, the ECG’s recorded P-waves, QRS complexes, and T-waves may be small, tall, wide, steep, or shallow. For example, the more the electricity moves away from an electrode, the more negative the wave—similarly, the slower the electricity moves, the wider the complexes.
An ECG reader should look at all of the waves and intervals and learn a system of interpretation. For example, most readers start by looking at heart rate, the rhythm, and then the waveform axis. They then examine the PR interval, QRS interval, and QT interval. Next, they look at the P-waves, Q-waves, QRS complexes, ST segments, and the T waves. Finally, they put this all together to make an ECG diagnosis and, more importantly, a clinical diagnosis.
ECG Vectors
ECG vectors represent the strength and direction of the electrical current. The higher a vector is, the more prominent it is on the ECG. As different cardiac tissue has its own electrical reading, you can calculate them to discover the mean vector or the average of their signal.
Each person has a unique mean vector based on their heart’s activity. Vectors typically flow from the upper right, down, and left. If a patient’s ECG shows an abnormal vector direction, this could signify underlying issues.
Combining the information about each wave’s direction and electricity strength, you can determine whether your patient’s health is ideal or if they need tests and treatment.
Putting It All Together
ECG interpretation is a complex subject, but before you can get started, it’s important to understand the basics of the tools you’re using. The next step is enrolling yourself in an ECG interpretation course like Executive Electrocardiogram Education.
ECGEDU.com offers a variety of online video courses that provide in-depth, easy-to-follow instruction on ECG interpretation. All of our courses are hosted by Dr. Scott Siegal and are designed to give the student a one-on-one feel.
Click here to learn about what’s included in our courses, or you can sign up for our ACLS Rhythms course absolutely free by clicking here.