During my internal medicine residency, one of our cardiologists would constantly pimp us on arrhythmias. We all had to memorize that arrhythmias were “abnormalities of impulse formation and/or conduction.” But, let’s get real – arrhythmias are simply abnormal heartbeats. There are many ways to classify arrhythmias, multiple means for diagnosing arrhythmias and numerous causes of arrhythmias. Learn how to diagnose, and classify cardiac arrhythmias. Also learn the symptoms, causes and tests for heart rhythm abnormalities. Here is a summary of arrhythmias, and what we look for.
Classification of Arrhythmias
Classifying arrhythmias may depend on your point of view at the time. For example it is always helpful to know if the arrhythmia is benign or life threatening as your patient’s life may depend on it. A provider may want to know where the arrhythmia originates – that is atrial or ventricular. You may classify it by its rate – that is brady-arrhythmia (slow heart rhythm) or tachy-arrhythmia (fast heart rhythm). Below are several ways to categorize arrhythmias:
- Benign vs. Life Threatening
- Atrial vs. Ventricular
- Supraventricular vs. Ventricular
- Right-sided vs. Left-sided
- Brady- vs. Tachy-
- Abnormality of Impulse Formation vs. Abnormality of Impulse Conduction
- Normal vs. Pathological
- Symptomatic vs. Asymptomatic

Different Arrhythmias
Despite making fun of my cardiology teacher, I will divide arrhythmias into abnormalities of impulse formation and abnormalities of impulse conduction.
Abnormalities of Impulse Formation
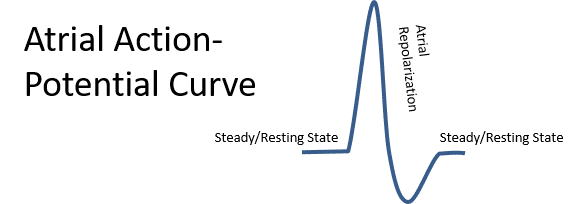
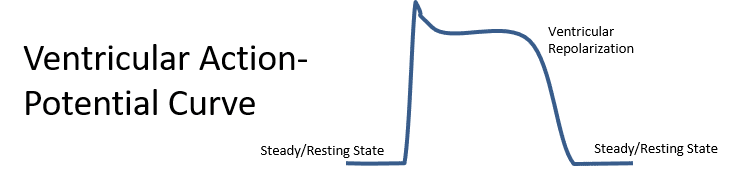
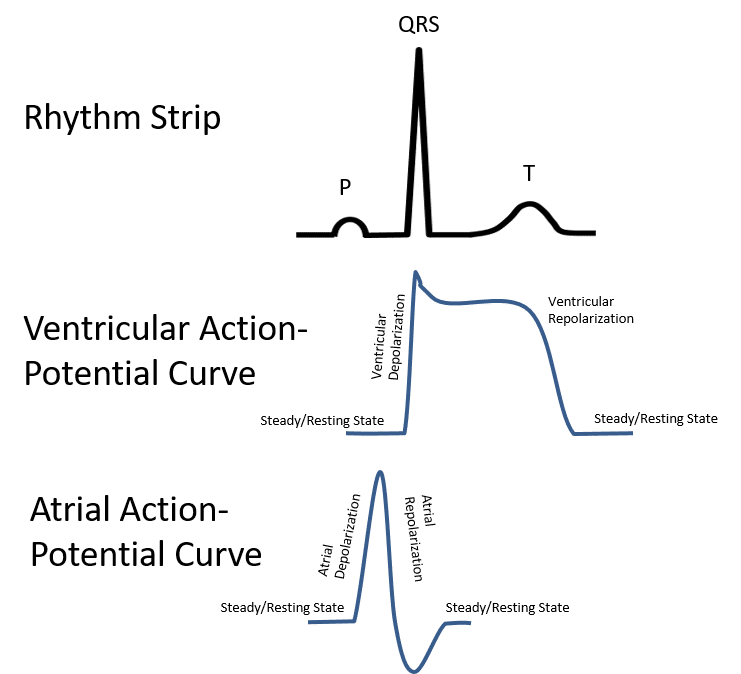
To comprehend impulse formation, we first need to understand the basics of action potential curve. To begin with, the tissue sits in a steady/resting state, based on ions and an intact cell membrane. A sufficient current then causes a voltage response, leading to depolarization. Other ionic changes occur causing repolarization of the cells until they return to their steady/resting state. Any alteration in this cycle, can lead to an arrhythmia.
You should also know that even though almost all-cardiac tissue is capable of generating impulses, most areas of the heart are stimulated by myocytes that generate an impulse first. For example, the sinoatrial (SA) node typically acts as the pacemaker of the heart. Impulses from the SA node then stimulate the atria, the atrioventricular (AV) node, and then the ventricles.
Electrocardiographic tracings, lines up with the action potential curve. P-waves occur due to depolarization of the sinus node and the atria. The QRS complex coincide with ventricular depolarization. The ST and T-wave represents repolarization of the ventricles. Since atrial repolarization occurs within the PR interval and the QRS complex, it is not easily recognized.
Examples of Abnormalities of Impulse Formation
The best-recognized, example of an abnormality of impulse formation is sinus tachycardia that occurs during exercise or stress. In this case, epinephrine (adrenaline) stimulates the sinoatrial node, which in turn makes the heart go faster. Similarly, when we are relaxed or sleeping, our heart rate slows. This is called sinus bradycardia. These are normal responses.
There are a slew of pathological abnormalities of impulse formation. A few examples are atrial fibrillation, supraventricular tachycardia (SVT), ventricular tachycardia, ventricular fibrillation, premature atrial complexes, and premature ventricular complexes.
Abnormalities of Impulse Conduction
Abnormalities of impulse conduction occur when an impulse cannot get through an area of the heart, or when there might be extra pathways (bypass tracts) that allow impulses to go through too easily.
Examples of Abnormalities of Impulse Conduction
At times, an impulse cannot get through an area of the heart. A good example of this is in third degree atrioventricular (complete) heart block. In this case, a section of the atrial ventricular (AV) node may not be functioning, which results in atrial impulses not conducting to the ventricle. A slower ventricular escape rhythm may then occur, as the ventricular tissue must rely on its intrinsic pacemaker characteristics. In some patients, there may be a block in one of the bundles, resulting in a right bundle branch block or a left bundle branch block. These too are defects of impulse conduction.
Some people are born with extra conduction pathways. These extra pathways conduct impulses aberrantly, causing certain arrhythmias. Examples of these might include atrioventricular nodal reentrant tachycardia or AVNRT (a type of supraventricular tachycardia), pre-excitation and/or Wolff-Parkinson-White syndrome, Lown-Ganong-Levine Syndrome. These are all reentrant-type of arrhythmias.
Symptoms of Arrhythmias
Arrhythmias can cause a multitude of symptoms. The most common symptom is palpitations or an irregular or peculiar beating of the heart. People describe palpitations differently. Some describe them as skipped beats, fluttering, pounding, slow beats, or an irregular heart rhythm. Patients may feel dizzy, lightheaded, or possibly faint. Some patients will get chest pain, sweating, or short of breath.
Causes of Arrhythmias
Arrhythmias can be from a normal process, a congenital abnormality, or brought on by external factors. As noted above, sinus tachycardia may be a normal response to stress or exercise. As also noted previously, some people are born with abnormal pathways within the heart that can cause arrhythmias. Damage to the heart from a heart attack, hypertrophy (thickening of the heart muscle), and further acquired conditions may foster arrhythmias. Other influences can promote or exacerbate arrhythmias. These may include alcohol, nicotine, caffeine, stimulants such as cocaine, certain medications, and electrolyte imbalances.
Testing For Arrhythmias
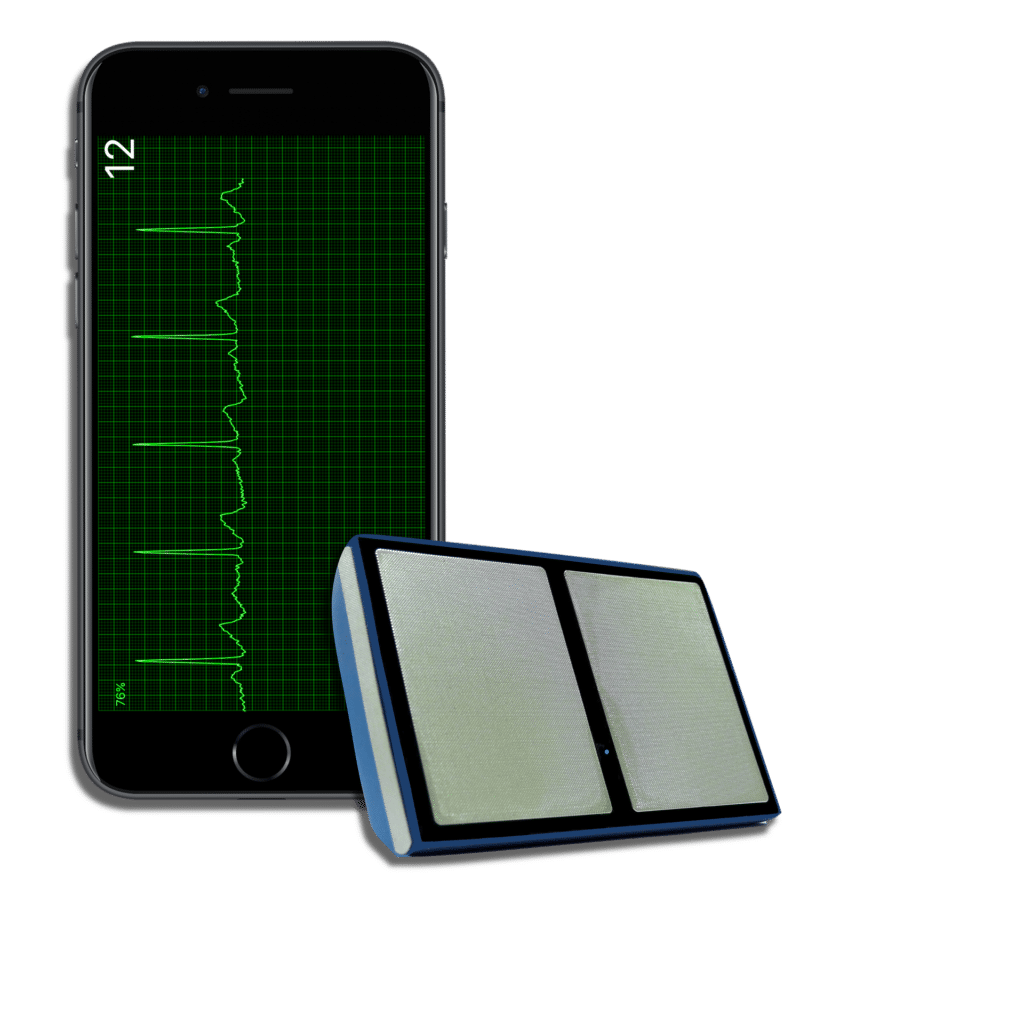
Identifying the abnormal heart rhythm, as well as the possible causes, typically requires testing. The first test is usually an electrocardiogram (ECG). ECGs may show the abnormal heart rhythm or cause such as an acute heart attack. Long-term cardiac monitors may be used. Patients typically wear these from 24 hours to 30 days. In some cases, an implantable device can monitor heart rhythms for years. Blood tests may detect electrolyte abnormalities, certain medication levels and illicit drugs. Echocardiograms (ultrasound of the heart) look for structural heart disease. Stress testing helps detect coronary artery disease (blockages in the arteries supplying the heart). In rare instances, patient receive a tilt table test, which looks for arrhythmia associated with changes in body position. Lastly, some patients require an electrophysiology study (study where wires in the heart guide the detection of arrhythmias).
How Do Medical Providers Learn To Diagnose Arrhythmias
Medical providers need to know how to diagnose arrhythmias. Courses on electrocardiogram (ECG) interpretation and identifying arrhythmias is standard in schools for clinicians and healthcare providers. Many providers certify in advanced cardiac life support (ACLS), where arrhythmia identification and management is part of the course. Currently, there are a lot of ECG books, college courses, and online resources that help.




