Almost all medical professionals require certification in Advanced Cardiac Life Support (ACLS) to work in the hospital or many medical facilities. Not only that, but they need to recertify in ACLS every two years. Trainees of ACLS learn how to treat cardiac emergencies like a myocardial infarction (heart attack), cardiac arrests, and life-threatening arrhythmias (abnormal heart rhythm). Additionally, providers learn to recognize and treat strokes, and other conditions that may lead to disability or death. This article helps you learn ACLS rhythms, terminology and definitions associated with the rhythms, and lastly the pathophysiology.

Clinical Algorithms
The mainstay of mastering ACLS is learning the algorithms associate with each medical condition. These algorithms show how to approach and treat cardiac arrest, bradycardia, tachycardia, acute coronary syndromes, and suspected strokes. Amongst these algorithms is the recognition and treatment o ventricular tachycardia, ventricular fibrillation, ventricular tachycardia (both with and without a pulse), asystole, and pulseless electrical activity (PEA).
Electrocardiogram Interpretation Skills
All students of ACLS learn to interpret basic cardiac arrhythmias or abnormal heart rhythms. Recognizing the abnormal rhythms is challenging for a lot of trainees. I find it best to understand the definitions, the pathology, and then recognize the arrhythmia. Sounds hard, but it really isn’t. Let’s go through some of this below. There are many fine resources for learning these arrhythmias. I put a free course together (ecgedu.com/ACLS) which quizzes students on the arrhythmias, and describes them in detail.
Terminology
If you are fluent in Latin or Greek, then skip this section. If not, here are some basic terms and how they are used with ECGs. More of these terms and definitions are available with ecgedu.com/arrhythmia course or in ecgedu.com/glossary.
ECG Definitions
- Normal: The heart rate related to 95% of the population. For example, Normal Sinus Rhythm describes a rhythm that originates from the sinus node at a rate between 60 and 100 beats per minute. In other words, 95% of people with sinus rhythm go between 60 and 100 beats per minute.
- Bradycardia: A heart rate less than normal. For example, a sinus rhythm <60 beats per minute is bradycardia.
- Tachycardia: A heart rate greater than 100 beats per minute.
- Flutter: A heart rate typically between 250 and 350 beats per minute. For example, atrial flutter refers to a fast atrial rhythm with atrial impulses occurring between 250 and 350 beats per minute. In atrial flutter, the ventricular rates are typically between 120 and 180 beats per minute. Remember don’t confuse the atrial rate with the ventricular rate.
- Fibrillation: A heart rate >350 beats per minute. For example, ventricular fibrillation describes quivering ventricles with ineffective ventricular impulses occurring at >350 beats per minute.
- Asystole: No heart rhythm
- Couplet: Two beats in a row. For example, two premature ventricular complexes in a row are called a ventricular couplet
- Sinus: Originating from the sinus node
- Junctional: Originating from the atrioventricular (AV) node (also known as the junction)
- Agonal: Relating to, or associated with the act of dying. For example, an agonal heart rhythm shows few ventricular beats suggesting minimal cardiac activity which is often a precursor of death.
- Supraventricular Tachycardia (SVT): Any rhythm originating from the upper chambers of the heart or the atrioventricular node that goes at a heart rate >100 beats per minute.
- Pulseless Electrical Activity (PEA): Seeing a rhythm on the ECG, but this electrical rhythm does not generate effective mechanical contraction of the heart muscle, therefore not giving a palpable pulse.
List of ACLS Rhythms
The ACLS rhythms taught include normal sinus rhythm, sinus bradycardia, sinus tachycardia, first degree atrioventricular (AV) block, second degree AV block, Mobitz type-1, and Mobitz type-2, third-degree AV block, atrial flutter, atrial fibrillation, supraventricular tachycardia, monomorphic ventricular tachycardia, polymorphic ventricular tachycardia, ventricular fibrillation, agonal rhythm, asystole, torsades de pointes.
Other rhythms that should be known include premature ventricular complexes, ventricular couplets multifocal atrial tachycardia, ectopic atrial rhythm, ventricular pacemaker rhythm, AV pacemaker rhythm, and Wolff Parkinson White.
Pathophysiology
Conduction typically begins in the sinoatrial (SA) node, goes to the atrioventricular (AV) node, and then into the ventricles. Arrhythmias are simply abnormalities in impulse formation or conduction. For example, in atrial arrhythmias such as atrial fibrillation, impulses begin from abnormal sites within the atria (top chambers of the heart). In ventricular arrhythmias such as ventricular tachycardia, impulses begin from abnormal foci within the ventricles (lower chambers of the heart).
Heart blocks and Wolff Parkinson White syndrome demonstrate abnormalities of conduction. During first, second, and third-degree atrioventricular (AV) blocks, conduction is slowed or halted within the AV node. The abnormalities seen on the ECG from Wolff Parkinson White occur due to an accessory pathway (extra channel for impulse conduction) that occurs between the atria and ventricles.
Learn ECG rhythm pathophysiology
ACLS Rhythms

Sinus Rhythms – Rhythms that originate from the sinus node
Normal Sinus Rhythm – heart rate 60-100 bpm
Sinus Bradycardia – heart rate < 60 bpm
Sinus Tachycardia – heart rate > 100 bpm
Atrial Rhythms – Rhythms that originate from a site(s) in the atria
Ectopic Atrial Rhythm – originates from one atrial site; heart rate 55-100 bpm
Multifocal Atrial Tachycardia – originates from multiple atrial sites; heart rate > 100 bpm
Atrial Flutter – originates from one atrial site; atrial rate 250-350 bpm; the ventricular rate varies (usually 120 -180 bpm)
Atrial Fibrillation – originates from multiple atrial sites; atrial rate >350 bpm; the ventricular rate varies (usually 120 -180 bpm)
Junctional (AV node) Rhythms – Rhythms that originate from the AV node (Junction)
Supraventricular Tachycardia (SVT) – usually refers to a narrow complex rhythm that originates from the AV node at a rate > 100 bpm.
Ventricular Rhythms – Rhythms that originate from a site(s) in the ventricles
Premature Ventricular Complexes (PVCs) – single early heartbeats that originate from the ventricle
Ventricular Couplets – two early extra beats together that originate from the ventricle
Ventricular Tachycardia
Monomorphic – originates from one ventricular site; ventricular complexes all look alike; the ventricular rate is > 100 bpm (usually 100-250 bpm)
Polymorphic – originates from multiple ventricular sites; ventricular complexes all look different; the ventricular rate is > 100 bpm (usually 100-250 bpm)
Torsades de Pointes – A subset of polymorphic ventricular tachycardia in which the ventricular complexes appear to get bigger and smaller in an ongoing pattern. This rhythm is associated with a prolonged baseline QT interval.
Agonal Rhythm – a slow irregular ventricular rhythm often associated with a dying heart
Asystole – no heart rhythm
Atrioventricular (AV) Blocks – delays or cessation of conduction through the AV node
First Degree AV Block – A benign delay in the conduction through the AV node
Second Degree AV Block
Mobitz Type-1 – A progressive fatiguing of conduction through the AV node until an impulse does not get through the AV node at all. The cycle repeats. This conduction abnormality is recognized by progressive lengthening of the PR interval and then an absent QRS complex.
Mobitz Type-2 – Intermittent and often unpredictable failure of conduction through the AV node. There are normal P waves followed by QRS complexes on some beats and then P waves without QRS complexes on other beats.
Third Degree (Complete) AV Block – Complete failure of conduction through the AV node. This results in a supraventricular rhythm (e.g. sinus rhythm) and a junctional or ventricular rhythm, each beating independently, but at the same time. In third-degree AV block, you see P waves marching out one after another with a constant cadence and QRS complexes marching out at their own cadence. The PR intervals all vary since there is no coordination between the atria and ventricles.
Wolff Parkinson White
During a sinus rhythm, the impulse can travel to the ventricle through an independent bypass tract, slightly before the impulse gets through the AV node. As such, the QRS complexes have a little slur (delta wave) on their front end. Additionally, the PR interval appears shorter than normal and the QRS complexes appear wider than normal. This abnormality may make patients prone to fast abnormal heart rhythms.
Pacemaker Rhythms
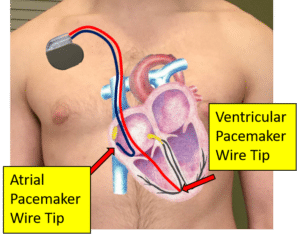
Rhythms produced by a small jolt of electricity from an implanted device that has a wire(s) in the heart. The heart rate depends on the rate programmed into the pacemaker.
Ventricular Pacemaker Rhythm – A rhythm produced by a device with a wire in the ventricle
Atrioventricular (AV) Pacemaker Rhythm – A rhythm produced by a device with wires in the atrium and ventricle.
Conclusion
To understand ACLS, medical professionals need to know the cardiovascular emergencies, and the algorithms to treat these emergencies. Additionally, students need to recognize certain cardiac arrhythmias and act appropriately. Mastering these arrhythmias is not hard, but requires knowing the terminology and particular rhythm patterns. Knowing the pathophysiology or processes associated with these rhythms is helpful, too. Hopefully, this article gave you some insight into these arrhythmias and ACLS protocols.




