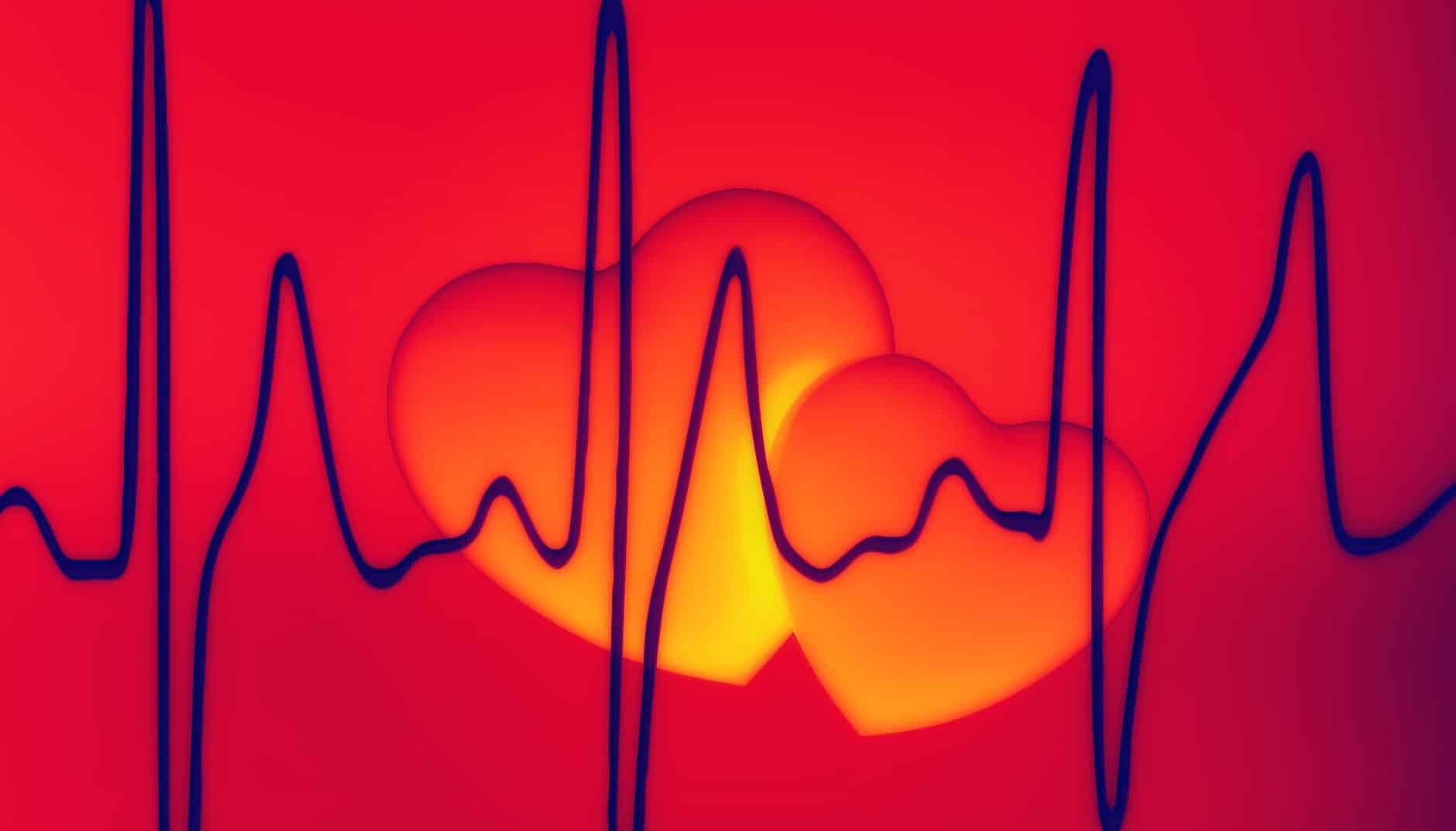
An arrhythmia is simply an abnormality of the rhythm of the heart. More specifically, it is an abnormality of cardiac impulse formation or conduction. That means that the areas of the heart that produce impulse may not function correctly leading to heart rhythms being too fast, too slow, or even cease. Additionally, an arrhythmia may affect the conduction of the electrical impulse. This too may cause abnormal heartbeats or rhythms that are too fast, or too slow. Some arrhythmias are insignificant whereas other arrhythmias are very serious and life-threatening. People with arrhythmias may feel palpitations. Arrhythmias are diagnosed using electrocardiograms (ECG), heart monitors, or on home rhythm monitoring devices.
Benign vs Dangerous Arrhythmias
Arrhythmias may be benign and clinically unimportant or may be serious and even life-threatening. The significance of the arrhythmia depends on which part of the heart it originates, the heart rate, and how it affects conduction through the heart.
Benign Arrhythmias
Benign arrhythmias are ones that do not clinically hurt the individual. Essentially they are harmless and do not threaten one’s health or life. Below are a couple of examples.
Sinus Tachycardia
Sinus tachycardia is a rhythm that originates from the sinus node, which is the normal pacemaker of the heart and goes faster than 100 beats per minute. This is a normal result of exercise, stress, or anxiety. Although classified as an arrhythmia this is normal, expected, and even desired in these conditions.
First-Degree Atrioventricular (AV) Block
A first-degree AV block is a minor conduction delay that occurs in the beginning portion of the atrioventricular node. The AV node is the area of the heart that connects the electrical system from the upper chambers of the heart (atria) to the lower chambers (ventricles). This delay may be caused by aging, enhanced vagal tone, heart attacks, electrolyte abnormalities, or medications. For the most part, no harm is caused to patients with first-degree AV blocks.
Premature Atrial Complexes
Premature atrial complexes (PAC) are extra, early beats that originate from the upper chambers of the heart. They may make the heartbeat feel irregular. They may occur rarely or frequently. Patients often describe a flip-flop sensation in their chest. The etiology is unknown, but they are typical in everyone and are benign.
Start Your Membership Today
We make electrocardiogram interpretation simple and understandable. The videos are interactive, and have detailed, easy to follow illustrations.
Dangerous Arrhythmias
As the word dangerous implies, these types of arrhythmias do cause injury to patients. This harm can come in the form of symptoms, like syncope (fainting), strokes, or even death. Below are a couple of examples of dangerous arrhythmias.
Atrial Fibrillation
Atrial fibrillation is an abnormal rhythm that originates from a multitude of hyperexcited sites within the upper chambers of the heart (atria). The foci give off 350-600 little jolts of electricity per minute causing the atria to quiver. All these jolts of electricity bombard the atrioventricular (AV) node. Fortunately, the AV node filters out most of these. Typically, 120-180 beats per minute get through. Some patients have palpitations, that is they feel their heart beating fast. Some feel nothing. Unfortunately, atrial fibrillation puts patients at risk of forming clots in the atria, which can then lead to a stroke.
Ventricular Tachycardia
Ventricular tachycardia (VT) is an abnormal rhythm that originates from the lower chambers of the heart (ventricles) and beats at a rate faster than 100 beats per minute. VT can cause the heart to beat inefficiently and impair blood circulation to the heart, brain, and other organs. The blood pressure may be low causing lightheadedness, fainting, shortness of breath, or congestive heart failure. This rhythm may degenerate to ventricular fibrillation and death. Causes of VT include structural heart disease from a heart attack or myocarditis, congenital cardiac abnormalities, electrolyte abnormalities, and adverse effects from some drugs, to name a few. These patients often need immediate treatment.
Complete Atrioventricular (AV) Block (aka Third-Degree Heart Block)
Certain conditions may cause the atrioventricular (AV) node to cease to function. When this happens, the electricity from the upper chambers of the heart (atria) cannot get to the lower chambers (ventricles). Often the intrinsic pacemaker characteristic of the ventricles takes over, which allows the ventricles to beat between 20 and 40 beats per minute. Unfortunately, this slow heart rate often leads to symptoms such as lightheadedness, dizziness, and syncope (fainting). This may also result in death. These patients need an urgent or emergent pacemaker placed. Complete heart block may be caused by damage to the AV node from surgery, a heart attack, or congenital abnormalities. It may also be caused by certain medications.
Example of Different Arrhythmias
Arrhythmias are named by where they originate and a comment about the rate. Other names may deal with delays in the conduction. First are some examples of arrhythmias based on where they originate in the heart. Next will be some arrhythmias based on conduction abnormalities.
Sinus Node Arrhythmias
- Sinus tachycardia – a rhythm originating from the sinus node at a rate > 100 beats per minute
- Sinus bradycardia – a rhythm originating from the sinus node at a rate < 60 beats per minute
- Sinus arrhythmia – a rhythm originating from the sinus node with a variable rate (typically at least a 0.16-second variation between the fastest and slowest beats)
- Sinus arrest – a long pause devoid of sinus beats (typically > 2 seconds)
Atrial Arrhythmias
- Ectopic atrial rhythm – a rhythm originating from the atria at a rate between 55 and 100 beats per minute (the rate reflects the atrial activity only; ventricular activity may have a different rate)
- Multifocal atrial tachycardia – a rhythm originating from the atria with atrial rates > 100 beats per minute, and at least 3 different looking P-waves suggesting at least 3 different atrial sites of origin.
- Atrial flutter – a rhythm originating from the atria with atrial rates of 150-250 beats per minute (ventricular rates will vary)
- Atrial Fibrillation – a rhythm originating from the atria with atrial rates > 350 beats per minute (ventricular rates will vary)
Atrioventricular (AV) Arrhtymias (aka Junctional Rhythms)
- Accelerated junctional rhythm – a rhythm originating from the atrioventricular (AV) node (junction) at a rate between 60 and 100 beats per minute
- Supraventricular tachycardia – a tachyarrhythmia that originates from the atria or AV node. This usually refers to rhythms that originate in the AV node and beat at rates > 100 beats per minute
Ventricular Arrhythmias
- Accelerated idioventricular rhythm (AIVR) – a rhythm originating from the ventricles at a rate between 40 and 100 beats per minute
- Ventricular tachycardia – a rhythm originating from the ventricles at a rate > 100 beats per minute
- Ventricular fibrillation – a rhythm originating from the ventricles with atrial rates > 350 beats per minute
Heart Blocks
- First degree atrioventricular (AV) Block – A slowing of the conduction from the atria to the ventricles through the atrioventricular (AV) node. PR interval > 0.2 seconds.
- Second degree atrioventricular (AV) block Mobitz Type 1 (Wenckebach) – A progressive slowing of the conduction from the atria to the ventricles through the atrioventricular (AV) node with an eventual interruption of atrial impulse conduction.
- Second degree atrioventricular (AV) block Mobitz Type 2: – A disorder of the atrioventricular (AV) node in which there is an intermittent complete failure of atrial impulses to conduct from the atria to the ventricles.
- Third degree atrioventricular (AV) block (complete heart block) – A disorder of the atrioventricular (AV node) in which there is a complete failure of atrial impulses to conduct from the atria to the ventricles.
Start Your Membership Today
We make electrocardiogram interpretation simple and understandable. The videos are interactive, and have detailed, easy to follow illustrations.
Symptoms From Arrhythmias
Not all patients have symptoms from arrhythmias. Symptoms may however include palpitations, chest pain, shortness of breath, anxiety, fatigue, dizziness, lightheadedness, fainting, or feeling faint. Palpitations are the perception or feeling that the heart is beating abnormally. Some describe them as a skipped beat, a dropped beat, a flip-flop in the chest or throat, or a sudden sinking sensation in the chest. Others note rapid beats, slow beats, flutters in the chest, and irregular heartbeats.
How to Detect Arrhythmias
The first thing that prompts doctors and other healthcare providers to look for arrhythmias is patient-reported symptoms. Sometimes, however, patients have no symptoms and an arrhythmia is detected by the provider noticing an irregular heartbeat during an examination. When an arrhythmia is suspected, the first test is an electrocardiogram (ECG or EKG). Often a longer-term cardiac monitor is performed. Patients wear these monitors for a prescribed period of time. They usually consist of two or more electrodes (sticky patches) connected to a monitor placed on the chest. They may be worn for 24 hours (Holter Monitor), 48 hours, weeks, or a month. Occasionally, a small monitor is implanted under the skin on the left side of the chest that will monitor the heart for years. This implantable loop recorder (ILR) is roughly 2 inches long and half the thickness of a pencil. Nowadays there are also cardiac monitoring devices on your phone or tablet.
Treatment of Arrhythmias
The treatment of arrhythmias depends on the type of arrhythmia and the severity of symptoms. Benign arrhythmias may be best treated by leaving them alone, patient education, and reassurance. Some arrhythmias require medications to control the heart rates or get rid of the abnormal beats. Other arrhythmias benefit from radiofrequency ablation. Ablation for simplicity is when a wire is placed inside the heart near the area causing the arrhythmia and electricity is applied which “burns” out the abnormality. Direct current cardioversion (applying a shock to the heart) is another possible treatment. This is used in emergent situations for severe arrhythmias like ventricular tachycardia, but can also be used as an outpatient treatment for other arrhythmias such as atrial fibrillation. Finally, some arrhythmias require a pacemaker or cardiac defibrillator.
Try Our ACLS Rhythm Course For Free!
This course goes through all of the ACLS rhythms. You will be quizzed on each rhythm and then watch the detailed description which points out the salient features.
How do I Learn About Arrhythmias
If you personally have palpitations or symptoms of an arrhythmia, then go see your provider. Learning the different arrhythmias requires training. ECG or arrhythmia courses are a good source. This is an important skill for any healthcare provider including doctors, nurse practitioners, and physician assistants. Nurses, emergency medical technicians (EMT), and anyone certifying in advanced cardiac life support (ACLS) also needs these skills.
Arrhythmias Made Simple from ecgedu.com makes arrhythmia interpretation understandable and straightforward. Our 2.25 hour online video course is self-paced and designed to give a one-on-one feel to learning arrhythmias. The videos are interactive and have easy-to-follow illustrations and examples. Sign up for our course now and see how easy learning arrhythmias really is. If you are not ready for this course, then sign up for our free ACLS rhythm course or watch a sample video to get a feel for our style and approach.